Cervical Cancer
Cervical cancer is a largely preventable and often treatable cancer, most commonly caused by persistent infection with high-risk human papillomavirus (HPV). Early detection through regular screening (Pap tests and HPV tests) greatly improves outcomes, and for some patients seeking cost savings or faster access to care, vetted medical tourism options can connect them with high-quality treatment and experienced specialists abroad. (See authoritative sources such as the National Cancer Institute for up-to-date guidance.)
Navigating Cervical Cancer: Your Guide to Treatment Options & Global Care
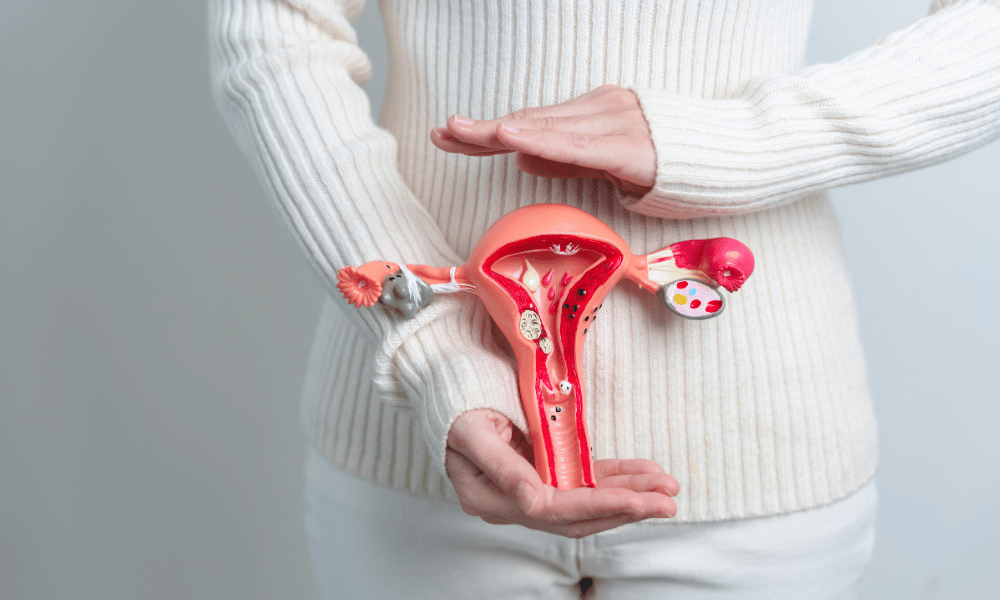
A diagnosis of cervical cancer can be overwhelming. Advances in screening, diagnosis, and care mean many people with cervical cancer now have effective treatment options and better outcomes than in the past. Cervical cancer begins in the cells of the cervix — the lower part of the uterus that connects to the vagina — and early detection is the single most important factor in improving prognosis.
What you’ll learn in this guide: how screening and tests detect abnormal cells early, what causes most cervical cancers, which treatment options are available by stage, and practical considerations if you’re exploring care at home or abroad. For authoritative, up-to-date information about causes and screening recommendations, consider resources such as the National Cancer Institute.
Most cervical cancers are linked to persistent infection with high‑risk human papillomavirus (HPV). Regular screening with Pap tests (Pap smears) and HPV tests can detect abnormal cells or HPV infection before cancer develops, and follow-up procedures like colposcopy and biopsy confirm a diagnosis when needed. If cancer is diagnosed, treatment is tailored to the individual — taking into account the stage, cancer type, overall health, and fertility goals — and may include local procedures, surgery, radiation, chemotherapy, targeted agents, or immunotherapy.
Globally, some patients also consider medical tourism to access timely, high-quality, and often more affordable cervical cancer treatment. This guide will help you compare screening and treatment pathways, understand options like bevacizumab or pembrolizumab for advanced disease, and evaluate safety and cost when researching hospitals abroad.
Understanding Cervical Cancer: What are the Symptoms to Watch For?
Early cervical cancer often causes no noticeable signs, which is why regular Pap tests and HPV testing are essential for detecting abnormal cells early. When symptoms do occur, they can include unusual vaginal bleeding, pelvic pain, or discomfort during sex — all of which warrant prompt medical evaluation.
A common question is “what are the warning signs of cervical cancer?” The reality: cervical cancer is frequently asymptomatic in its early, most treatable stages. Screening tests such as the Pap smear and HPV test detect abnormal cells or high‑risk HPV infections before cancer develops. If you do notice symptoms, don’t ignore them — early assessment and testing improve treatment options and outcomes. For authoritative guidance on screening intervals and follow-up, consult resources like the National Cancer Institute.
Red flags and common symptoms to watch for:
- Unusual vaginal bleeding: Bleeding after intercourse, between periods, after menopause, or heavier-than-normal bleeding — frequently reported and one of the most common signs prompting evaluation.
- Unusual vaginal discharge: Watery, bloody, thick, or foul‑smelling discharge that is new or persistent.
- Pelvic pain or pain during intercourse: New or worsening pain not related to your menstrual cycle.
- Painful or frequent urination: Can occur if the disease involves the bladder.
- Swelling in one leg: May indicate advanced disease affecting lymphatic drainage or blood flow.
- Unexplained weight loss or fatigue: General signs that can accompany many cancers.
When to see a doctor: contact your healthcare provider promptly if you experience any red-flag symptoms — especially postcoital bleeding, bleeding after menopause, or persistent pelvic pain. Your provider may recommend a Pap test (Pap smear), HPV test, or refer you for colposcopy and biopsy to evaluate abnormal cells. Remember: many benign conditions can cause similar symptoms, but prompt evaluation ensures abnormal cells are found early and managed effectively.
What Causes Cervical Cancer and Who is at Risk?
Persistent infection with high‑risk types of human papillomavirus (HPV) is the primary cause of cervical cancer. Other factors can increase the likelihood that an HPV infection progresses to cancer, including immune suppression, smoking, and certain reproductive and behavioral factors.
People often ask “what causes cervical cancer?” — the short answer: most cervical cancers are linked to long‑term infection with high‑risk HPV types. HPV is a very common sexually transmitted virus; in most people the infection clears on its own, but persistent infection with high‑risk strains can cause abnormal changes in the cells of the cervix (the lower part of the uterus) that may progress to cancer over years. For up‑to‑date statistics and guidance, consult authoritative sources such as the National Cancer Institute or WHO.
Beyond HPV infection, several risk factors are associated with a higher chance that abnormal cervical cells will develop into cancer:
- Weakened immune system: Conditions like HIV or use of immunosuppressant drugs reduce the body’s ability to clear HPV infections.
- Smoking: Tobacco exposure is linked to higher cervical cancer risk; toxins in tobacco can damage cervical cells and impair local immune response.
- Sexually transmitted infections: Co‑infections such as chlamydia have been associated with increased risk in some studies, though HPV remains the central cause.
- Reproductive factors: Long‑term use of oral contraceptives, multiple full‑term pregnancies, and early age at first full‑term pregnancy have been linked to modest increases in risk in some analyses.
- Lifestyle and socioeconomic factors: Poor diet, obesity, and limited access to regular screening (Pap tests / Pap smears and HPV testing) can contribute to higher risk and later detection.
What you can do to reduce risk: get the HPV vaccine according to current recommendations, practice safer sex, stop smoking, and keep up with regular cervical cancer screening (Pap smear and HPV test) so that abnormal cells are detected and treated early. These prevention steps are proven to lower rates of cervical cancers and improve outcomes — see the National Cancer Institute for vaccination and screening guidelines.
Exploring Cervical Cancer Treatment Options: What Procedures are Available?
Treatment for cervical cancer depends on the stage and goals of care — from conservative procedures that remove abnormal cells to major surgery, radiation, chemotherapy, and newer targeted or immunotherapies for advanced disease. Decisions are individualized and made by a multidisciplinary team.
Patients commonly ask “what are the treatment options for early stage cervical cancer?” or “can cervical cancer be cured?” When detected early, many cervical cancers are highly treatable and often curable. Treatment choice is guided by the cancer’s stage, the tumor type, the patient’s overall health, and fertility preferences. Below is an organized overview of common procedures and therapies, with the typical treatment goal noted (curative vs. organ preservation vs. symptom control).
For Precancerous Cells and Early (Stage I) Disease — organ‑sparing and curative options
- LEEP (Loop Electrosurgical Excision Procedure): An outpatient procedure using a heated wire loop to excise abnormal cervical tissue. Goal: remove abnormal cells and preserve the uterus.
- Cold‑knife conization (cone biopsy): A cone‑shaped tissue sample is removed for diagnosis and treatment; provides a more complete specimen for pathology than LEEP. Goal: diagnostic and potentially curative for small lesions.
- Cryosurgery and laser ablation: Minimally invasive techniques that destroy abnormal surface cells; typically reserved for selected precancerous lesions. Goal: local treatment with minimal recovery time.
For Invasive Cervical Cancer — curative or multimodal approaches
- Hysterectomy (radical hysterectomy): Removal of the uterus, cervix, part of the vagina, and nearby tissues including pelvic lymph nodes; may be performed open, laparoscopically, or robotically. Goal: curative for many early invasive cancers.
- Trachelectomy (fertility‑sparing): Removes the cervix and surrounding tissue while preserving the uterus for selected early‑stage patients who wish to retain fertility. Goal: cure while preserving childbearing potential (appropriate patient selection is critical).
- Radiation therapy: External beam radiation and brachytherapy (internal radiation) are used alone or with chemotherapy, especially for locally advanced disease. Goal: curative or palliative depending on stage.
- Chemotherapy: Systemic drugs are used with radiation (concurrent chemoradiation) or alone for advanced disease. Goal: eradicate microscopic disease, improve radiation effectiveness, or control metastatic disease.
- Targeted therapy: Agents that attack specific tumor pathways. Example: bevacizumab (Avastin) is used in certain advanced or recurrent cervical cancer regimens; discuss indications with your oncologist. Goal: improve outcomes in advanced disease.
- Immunotherapy: Checkpoint inhibitors such as pembrolizumab (Keytruda) may be an option for some patients with advanced or recurrent disease whose tumors express certain biomarkers. Goal: control disease when other therapies have been exhausted.
Treatment planning should involve a gynecologic oncologist, medical oncologist, and radiation oncologist. Which option is “best” depends on tumor type (most are squamous cell carcinoma or adenocarcinoma), exact stage, imaging and pathology findings, and patient priorities such as fertility. For current guideline recommendations and staging‑based treatment algorithms, consult resources such as the National Cancer Institute or professional societies (ASCO, NCCN).
Example (fertility preservation): a young patient with a small, early lesion on the cervix may be a candidate for conization or trachelectomy instead of hysterectomy — but this requires careful staging and specialist consultation. Your multidisciplinary team will explain risks, benefits, and expected recovery for each procedure.
Am I a Candidate for Cervical Cancer Treatment? Eligibility & Staging Explained
Eligibility for specific cervical cancer treatments depends primarily on the cancer’s stage (commonly classified using the FIGO staging system), the tumor type, the patient’s overall health and co‑existing conditions, age, and whether fertility preservation is desired. Early, localized cancers usually have more conservative or surgical options, while advanced disease often requires combined systemic and local therapies.
A key question after diagnosis is “who is eligible for which treatment?” The most important determinant is stage. The FIGO staging system (used internationally) classifies cervical cancer from Stage I (disease confined to the cervix) through Stage IV (spread to distant organs). Treatment recommendations follow staging but are individualized based on diagnostic tests, imaging, and patient goals.
- Stage I: Cancer limited to the cervix — options often include LEEP, conization, radical hysterectomy, or fertility‑sparing trachelectomy for carefully selected patients.
- Stage II: Disease beyond the cervix but not to the pelvic wall or lower third of the vagina — treatments typically involve radical hysterectomy with possible adjuvant radiation/chemotherapy, or definitive chemoradiation as the primary approach.
- Stage III: Spread to the lower third of the vagina, pelvic sidewall, or causing hydronephrosis — concurrent chemoradiation is commonly recommended.
- Stage IV: Distant spread to organs such as bladder, rectum, lungs, or bones — treatment focuses on systemic therapy (chemotherapy, targeted agents, immunotherapy) and palliative measures to manage symptoms.
Other factors that affect eligibility:
- Overall health and comorbidities: Heart, lung, kidney function and other conditions influence tolerance for surgery, chemotherapy, or radiation.
- Age: Chronological age alone is not a barrier, but older patients may require tailored approaches based on fitness and co‑morbidities.
- Desire for fertility: For select early‑stage patients who want future pregnancy, fertility‑sparing procedures (e.g., trachelectomy) may be offered after careful evaluation.
- Cancer type and pathology: Most are squamous cell carcinomas, but adenocarcinomas and rarer histologies can affect treatment planning.
A complete evaluation by a gynecologic oncologist usually includes a physical exam, biopsy results, and imaging (MRI, CT, or PET) to determine stage and guide therapy. Whenever possible, ask for care planning by a multidisciplinary tumor board and consider a second opinion to confirm the diagnosis and recommended cervical cancer treatment. For staging details and guideline‑based algorithms, refer to FIGO and resources such as the National Cancer Institute.
Navigating Recovery: What to Expect After Cervical Cancer Treatment?
Recovery after cervical cancer treatment varies by the procedure: minimally invasive procedures usually allow a faster return to daily life, while radical surgery or combined chemoradiation require longer healing and attention to potential long‑term effects. Your care team will tailor recovery guidance to your treatment, overall health, and goals.
Patients often ask, “how long is recovery after hysterectomy?” or “what is life like after treatment?” Recovery is a process that includes physical healing, emotional adjustment, and monitoring for side effects. Below are typical timelines, common expectations, and practical tips to help you plan and manage recovery.
Quick reference — typical recovery windows
- 0–2 weeks: Recovery from outpatient procedures (LEEP, cryotherapy) with light activity recommended.
- 2–8 weeks: Healing after minimally invasive hysterectomy; many return to normal activities in this window.
- 6–12+ weeks: Full recovery after open radical surgery can take this long; chemoradiation recovery may extend months due to cumulative side effects.
Recovery after Localized Procedures (LEEP, Conization, Cryosurgery, Laser Ablation)
- Duration: Usually a few days to a couple of weeks.
- Expectations & practical tips: Mild cramping, light spotting, or watery discharge are common. Avoid tampons, douching, and sexual intercourse for the timeframe advised by your doctor. Plan for a day or two off work and arrange support for errands if needed.
Recovery after Hysterectomy (including Radical Hysterectomy)
- Duration: Typical hospital stay 2–5 days. Full recovery: 6–8 weeks after open surgery, or 2–4 weeks after minimally invasive approaches.
- Expectations & practical tips: You will need pain control, progressive activity (short walks), and help with heavy lifting for several weeks. Emotional impacts (body image, fertility loss) are common — seek counseling or support groups. Discuss contraception, hormone management, and fertility options beforehand if relevant.
Recovery after Radiation Therapy
- Duration: Side effects often peak during treatment and may persist for weeks to months; some long‑term effects can last years.
- Expectations & practical tips: Fatigue, skin changes, bowel/bladder irritation, and vaginal dryness or narrowing can occur. Ask your team about pelvic floor therapy, vaginal dilators to prevent stenosis, and strategies to manage bowel/bladder symptoms.
Recovery after Chemotherapy
- Duration: Side effects are most intense during cycles but often improve between cycles; fatigue can linger for months after treatment ends.
- Expectations & practical tips: Nausea, hair loss, mouth sores, infection risk, and neuropathy are possible. Maintain nutrition, follow antiemetic plans, monitor blood counts, and report fevers promptly to your doctor.
Recovery support and follow‑up: regular follow-up appointments, surveillance tests, and imaging are essential to monitor for recurrence and manage long‑term effects. Practical supports — physical therapy, pelvic floor rehab, fertility counseling, and psychosocial services — can improve quality of life during survivorship. Always discuss timelines for safe travel, work return, and sexual activity with your treating doctor.
What are the Potential Risks and Side Effects of Cervical Cancer Treatments?
Treatments for cervical cancer can cause short‑term effects such as pain, bleeding, nausea, and fatigue, and in some cases lead to long‑term issues including infertility, lymphedema, bowel or bladder dysfunction, and vaginal changes. The specific risks vary by procedure and by individual factors; your care team will discuss expected side effects and management strategies before treatment.
Patients frequently ask, “is cervical cancer treatment painful?” and “what long‑term effects should I expect?” While pain and discomfort are common shortly after procedures, most side effects can be managed. Below is a concise, stage‑and‑procedure‑oriented breakdown of typical short‑term and long‑term risks and practical tips for management. For drug‑specific risks (for example, targeted agents or immunotherapies), ask your oncologist for current prescribing information and guidance.
Localized Procedures (LEEP, Conization, Cryotherapy, Laser)
- Short‑term: Mild cramping, light bleeding or watery discharge, and a small infection risk. Most symptoms resolve in days to weeks.
- Long‑term: Possible cervical stenosis (narrowing) that may affect menstruation or fertility and a small increased risk of preterm birth after deep conization.
Hysterectomy (including Radical Hysterectomy)
- Short‑term: Pain, bleeding, wound infection, and rare injury to nearby organs (bladder, bowel, ureters); risk of blood clots during recovery.
- Long‑term: Permanent loss of fertility if the uterus is removed, potential lymphedema after lymph node removal, bladder or bowel changes, vaginal shortening or dryness, and surgical menopause if ovaries are removed.
Radiation Therapy (External Beam and Brachytherapy)
- Short‑term: Fatigue, localized skin irritation, bowel or bladder irritation (diarrhea, urgency), and vaginal soreness or discharge.
- Long‑term: Chronic bowel or bladder dysfunction, vaginal stenosis and pain with intercourse, lymphedema, and in rare cases risk of radiation‑related secondary malignancies.
Chemotherapy
- Short‑term: Nausea, vomiting, fatigue, hair loss, mouth sores, low blood counts (infection risk, bleeding, anemia).
- Long‑term: Peripheral neuropathy (nerve damage), possible heart or kidney effects with certain agents, premature menopause and infertility, and cognitive changes (“chemo brain”).
Targeted Therapy and Immunotherapy
- Targeted therapy (e.g., bevacizumab): Can cause high blood pressure, bleeding, clotting, protein in the urine, and rarely serious events such as gastrointestinal perforation. Regular monitoring is required.
- Immunotherapy (e.g., pembrolizumab): May trigger immune‑related adverse events where the immune system inflames healthy organs (lungs, colon, liver, endocrine glands). Symptoms can include fatigue, rash, diarrhea, cough, or shortness of breath and require prompt management.
When to Contact Your Care Team
Seek urgent medical attention for fever after chemotherapy, heavy bleeding, severe uncontrolled pain, sudden swelling or shortness of breath, or any new neurologic symptoms. For immune‑related symptoms on immunotherapy, report signs early so treatment (often steroids) can prevent serious complications.
Your oncology team will provide specific instructions on symptom management, follow‑up testing, and supportive care (nutrition, pelvic floor therapy, lymphedema management, fertility counseling). For the latest evidence and drug‑specific safety information, consult your treating physician and reputable sources such as drug labels and professional guidelines.
Worldwide Cervical Cancer Treatment Costs: Where Can You Find Affordable Care?
Cervical cancer treatment costs vary widely by country, stage, and the mix of services needed — from outpatient procedures to complex multimodality care. Many medical‑tourism destinations (for example, Mexico, India, Thailand, and Turkey) can offer comparable cancer treatment quality at lower total costs, but estimates depend on what is included (surgeon and hospital fees, implants, drugs, imaging, and length of stay).
Cost is a top concern for patients and families. In countries like the United States, comprehensive cervical cancer care (surgery, radiation, chemotherapy, and targeted/immunotherapy when needed) can be expensive, prompting some people to compare domestic care with international options. The true cost depends on the stage of disease, required procedures and therapies, pre‑ and post‑operative testing, hospital stay length, and whether advanced drugs (targeted agents or immunotherapies) are used.
Below is a general, illustrative cost comparison. These are estimates only (prices change by year and facility). Always request a detailed, itemized quote that states what is included (surgeon fee, anesthesia, pathology, implants, prostheses, inpatient days, medications, follow‑up visits, and any additional diagnostics).
| Procedure TypeUSA (Estimated Range)Medical Tourism Destinations (Estimated Range) | ||
| LEEP / Conization (Outpatient) | $2,000 – $8,000 | $500 – $2,500 (Mexico, India, Turkey) |
| Radical Hysterectomy (Open) | $30,000 – $70,000+ | $8,000 – $25,000 (Mexico, India, Thailand, Turkey) |
| Radical Hysterectomy (Laparoscopic / Robotic) | $40,000 – $90,000+ | $12,000 – $35,000 (Mexico, India, Thailand, Turkey) |
| Radiation Therapy (External Beam, per course) | $20,000 – $50,000+ | $5,000 – $15,000 (India, Thailand, Turkey) |
| Chemotherapy (per cycle; drug costs vary) | $5,000 – $20,000+ | $1,000 – $5,000+ (India, Mexico, Turkey) |
| Combined Chemoradiation (full course) | $60,000 – $150,000+ | $15,000 – $40,000+ (India, Thailand, Turkey) |
| Targeted Therapy / Immunotherapy (per cycle; drug costs vary) | $10,000 – $30,000+ | $3,000 – $10,000+ (India, Turkey, some European centers) |
These ranges are illustrative and should be treated as estimates. When comparing options, ask potential hospitals for (1) a dated, itemized quote, (2) details about included diagnostics and follow‑up, (3) accreditation and surgeon credentials (e.g., JCI), and (4) patient outcome data when available. A medical tourism facilitator or the hospital’s international patient office can often provide transparent cost breakdowns and logistics support.
Why Consider Cervical Cancer Treatment Abroad? Unlocking Global Healthcare Value
Seeking cervical cancer treatment abroad can provide meaningful value: lower overall costs for comparable care, access to advanced technology and specialized teams, shorter wait times in many centers, and tailored international patient services that support logistics and recovery.
For some patients facing high domestic costs or long delays for cancer treatment, medical tourism becomes a practical option. Beyond price, factors that drive people to consider care overseas include availability of specific procedures or technologies, experienced gynecologic oncology teams, and coordinated international patient programs that simplify travel, translation, and post‑op support.
Key potential benefits:
- Cost savings: Many international centers offer treatments at substantially lower prices than in North America or Western Europe — illustrative savings can be large, but exact percentages vary by procedure and must be verified with itemized quotes.
- Access to advanced treatments and technology: International hospitals often invest in modern equipment (robotic surgery, advanced radiation platforms) and have specialists trained in high‑volume centers.
- Reduced wait times: Faster scheduling for consultations, diagnostics, and surgery can be critical when timely treatment matters.
- Specialized expertise and international patient support: Dedicated gynecologic oncology teams and international patient offices can help coordinate care, visas, accommodation, and follow‑up.
- Privacy and a healing environment: Some patients prefer the discretion of receiving care away from home and appreciate recovery in a supportive setting.
Balance the benefits with potential downsides
- Continuity of care: Plan how follow‑up and any complications will be managed once you return home; coordinate with your local doctor before travel.
- Quality verification: Confirm hospital accreditation (e.g., JCI), surgeon credentials, and review outcome data or patient testimonials.
- Logistics and risk: Consider travel safety after major procedures, visa requirements, travel insurance that covers medical complications, and language support.
If you’re considering treatment abroad, request a dated, itemized treatment plan and quote, verify accreditation and surgeon experience, and ask about post‑treatment follow‑up and communication with your local doctor. For guidance on screening, diagnosis, and standard treatment pathways, consult trusted resources such as the National Cancer Institute.
Which Countries Offer the Best Value for Cervical Cancer Treatment?
Several countries are known for offering high‑value cervical cancer care — combining experienced specialists, modern facilities, and international patient services with prices that are often lower than in Western markets. Popular destinations include India, Thailand, Turkey, Mexico, and South Korea, each with distinct strengths in oncology services and patient support.
When evaluating “best countries for cervical cancer treatment,” look beyond price. Consider hospital accreditation (e.g., JCI), surgeon credentials, available technology (robotic surgery, advanced radiation platforms), international patient departments, and follow‑up care arrangements. Below are concise, practical notes about commonly chosen destinations and what they typically offer.
- India: Strengths — affordability, large volume of oncology cases, many specialists trained in Western centers, and numerous JCI‑accredited hospitals in cities like Delhi, Mumbai, Chennai, and Bangalore. Ideal for comprehensive care from diagnostics to complex surgery, radiation, and chemotherapy at competitive pricing.
- Thailand: Strengths — excellent medical infrastructure, strong hospitality services, and internationally recognized hospitals (especially in Bangkok). Patients often report high levels of international patient support and comfortable recovery environments.
- Turkey: Strengths — strategic location for European and Asian patients, significant investment in healthcare technology, and many JCI‑accredited centers in Istanbul and Ankara. Competitive pricing and experienced multidisciplinary oncology teams are common.
- Mexico: Strengths — geographic proximity for North American patients, bilingual staff in many centers, and modern hospitals in cities like Tijuana, Guadalajara, and Mexico City. Good option for outpatient procedures and shorter hospital stays.
- South Korea: Strengths — cutting‑edge technology and highly efficient hospital systems; while costs may be higher than India or Thailand, outcomes and technology availability are often excellent, particularly for complex diagnostic and surgical care.
Actionable tips when choosing a hospital abroad: request surgeon CVs and outcome data, confirm JCI or equivalent accreditation, ask for an itemized, dated quote, verify availability of an international patient coordinator, and check visa and expected stay requirements for treatment and recovery. Coordinate with your local doctor to ensure continuity of care and a clear follow‑up plan after you return home. For up‑to‑date guidance on screening, diagnosis, and treatment standards, consult reputable sources such as the National Cancer Institute.
What to Expect When Traveling for Cervical Cancer Treatment Overseas?
Traveling for cervical cancer treatment requires careful planning: choose a reputable provider, organize medical records and travel documents, arrange accommodation and local support, and prepare for consultations, the procedure itself, and follow‑up care. Good planning reduces stress and helps ensure continuity of care.
If you’re considering medical tourism for cervical cancer, here’s a practical, step‑by‑step overview of the typical process and what to prepare. Confirm details with the hospital’s international patient office and your local doctor, and check up‑to‑date visa and travel advisories for your destination.
- Initial consultation & planning:
- Research hospitals and doctors: Verify accreditation (for example JCI), surgeon credentials, and patient outcomes. Request surgeon CVs and ask about experience with cervical cancer treatment.
- Prepare medical records: Compile Pap test results, HPV test reports, biopsy pathology, imaging (MRI/CT/PET), and prior treatment notes. Electronic copies and a concise medical summary will speed remote review.
- Remote consultation & quote: Many centers offer virtual consultations to review your case, propose treatment options, and provide an itemized treatment plan with estimated length of stay and costs.
- Travel logistics & documentation:
- Visas & passport: Ensure your passport is valid and apply for any required medical visa well in advance.
- Flights & accommodation: Book flights and arrange lodging near the hospital. Many hospitals or facilitators can recommend vetted hotels and recovery‑friendly options.
- Insurance & travel coverage: Purchase travel insurance that covers medical complications and check whether your health insurance offers any overseas benefits. Clarify payment terms and refund policies with the hospital.
- Language & support: Confirm availability of English‑speaking staff or translation services, and note emergency contact numbers and the international patient coordinator’s details.
- Arrival, in‑person evaluation & treatment:
- Airport pick‑up & orientation: Many hospitals arrange transfers and an initial orientation with the international patient team.
- Confirmatory diagnostics: Expect in‑person consultation and possible repeat tests (imaging, labs, biopsy review) to finalize staging and the exact treatment plan.
- Undergoing treatment: Receive the agreed treatment (e.g., LEEP, surgery, radiation, chemotherapy). Ask for clear discharge instructions and a written follow‑up schedule before leaving the hospital.
- Recovery period: Plan to remain at least the minimum recommended time for post‑op recovery before travel; some procedures or complications require longer local recovery.
- Post‑treatment follow‑up & returning home:
- Discharge instructions: Obtain detailed, dated instructions for wound care, medications, activity restrictions, and emergency contacts.
- Follow‑up plan: Establish how follow‑up will be handled (virtual visits with the overseas team, coordinated care with your local doctor, timing of surveillance tests such as Pap test or imaging).
- Safe travel home: Confirm you are medically fit to travel; get documentation for airlines if needed and plan medical escorts for higher‑risk cases.
Practical checklist to bring: copies of Pap smear and HPV test results, biopsy and pathology reports, imaging files (MRI/CT/PET on USB or cloud link), current medications list, a short medical summary, and emergency contact and insurance details. Ask the hospital for a checklist and consider using a reputable medical tourism facilitator to coordinate logistics.
Finally, coordinate care with your local doctor before travel and confirm how they will be involved in post‑treatment surveillance. For guidance on screening tests, diagnostic pathways, and recommended follow‑up intervals, trusted resources such as the National Cancer Institute provide up‑to‑date recommendations.
How to Ensure Safety and Quality for Cervical Cancer Treatment Abroad?
To maximize safety and quality when seeking cervical cancer care overseas, verify hospital accreditation, confirm surgeon credentials and experience, review patient outcomes and testimonials, insist on transparent treatment plans and itemized costs, and use reputable international patient services or facilitators to coordinate logistics and continuity of care.
Quality and safety are paramount when choosing care for a serious condition like cervical cancer. Below is a practical checklist and the key questions to ask so you can evaluate providers confidently and reduce risks associated with medical travel.
- Check accreditation and standards: Look for Joint Commission International (JCI) accreditation or equivalent national accreditation. Accreditation indicates adherence to international quality and safety benchmarks; verify the hospital’s accreditation on the accreditor’s website.
- Verify doctor and team credentials: Request the gynecologic oncologist’s CV, board certifications, and experience with the specific cervical cancer type and procedures you need. Ask how many similar procedures the surgeon performs annually.
- Ask for outcome data and patient references: Request anonymized outcome statistics (complication rates, survival where appropriate) and read verified patient testimonials. Consistent positive outcomes are a stronger signal than isolated reviews.
- Demand transparent treatment plans and itemized costs: Obtain a dated, written treatment plan that lists all expected services and an itemized quote covering surgeon fees, anesthesia, hospital stay, imaging, pathology, medications, and follow‑up visits. Clarify refund and complication policies.
- Confirm technology and protocols: Ask which diagnostic and treatment technologies are available (MRI, PET, robotic surgery, modern radiation platforms) and whether the hospital follows internationally recognized treatment guidelines.
- Understand communication and international patient support: Ensure the hospital has an international patient office, named points of contact, language assistance, and clear processes for remote follow‑up and medical record transfer to your local provider.
- Review emergency and complication protocols: Ask how complications are handled, where emergency care is provided, and whether the hospital will coordinate care with local specialists if prolonged treatment is required.
- Use reputable facilitators carefully: Medical tourism facilitators can streamline logistics and vet options, but verify the facilitator’s reputation, ask if they have conflict‑of‑interest disclosures, and independently confirm any claims they provide.
- Get a second opinion: Before finalizing major treatment, obtain a second opinion—either locally or from another international specialist—to confirm staging, diagnosis, and the proposed cervical cancer treatment plan.
Practical next steps: prepare a concise medical packet (Pap/HPV test results, biopsy/pathology, imaging, medication list) to share during remote consultations; request surgeon CVs and outcome data; ask for an itemized, dated quote; and confirm post‑treatment follow‑up arrangements with both the overseas team and your local doctor. Doing thorough research and due diligence will help ensure the highest possible quality of care.
What are Patient Success Stories and Testimonials from Abroad?
Many cervical cancer patients report positive outcomes after receiving care abroad, citing affordable, high‑quality treatment and supportive specialty teams in countries such as India, Thailand, Mexico, and Turkey. These anonymized examples illustrate how careful planning and vetted providers can deliver timely, effective care.
Reading patient stories can help you understand real‑world experiences when considering medical tourism for cervical cancer. Keep in mind that these are individual experiences — outcomes vary — and thorough vetting of hospitals, surgeons, and aftercare plans remains essential.
Example 1: Maria from Canada (Hysterectomy in Mexico)
Maria had Stage IB cervical cancer and faced long surgical wait times at home. After researching accredited hospitals and surgeon experience, she chose a modern hospital in Mexico City. “The surgery went smoothly, the team communicated clearly, and my recovery was closely monitored. The total cost was substantially lower than private care at home, and I felt supported throughout.”
Example 2: Sarah from the UK (Chemoradiation in India)
Sarah required complex chemoradiation and advanced brachytherapy. She consulted with a leading cancer center in Chennai after comparing treatment timelines and costs. “The multidisciplinary team coordinated my radiation and chemo seamlessly. The technology and expertise were excellent, and the cost was much more manageable than private alternatives back home.”
Example 3: Emily from the USA (LEEP procedure in Turkey)
Emily found high‑grade precancerous cells and faced high out‑of‑pocket costs. She selected a JCI‑accredited clinic in Istanbul for a LEEP procedure. “From the virtual consult to discharge, everything was professional. The doctor explained risks and follow‑up clearly, and the overall process was cost‑effective and reassuring.”
What these examples teach us: verify hospital accreditation and surgeon experience, request an itemized cost and recovery plan, confirm international patient support and language services, and plan for coordinated follow‑up with your local doctor. Remember to balance hopeful testimonials with realistic expectations — not every case will mirror these outcomes, and complications can occur. Always seek second opinions for major treatment decisions and consult trusted sources for screening and treatment standards, such as the National Cancer Institute.
Take the Next Step with DGS Healthcare
Ready to explore safe, accredited treatment options abroad for cervical cancer? Compare top clinics, get an itemized quote tailored to your diagnosis and stage, and receive confidential guidance on screening, prevention, and travel logistics. No obligation — accredited partners and patient privacy protected.
Have questions right now? Call our international patient team or use live chat for urgent inquiries.
DGS Healthcare connects you with verified hospitals and specialists; discuss prevention, HPV vaccination, and follow‑up care with your care team. For screening and clinical guidance, see authoritative sources such as the National Cancer Institute.
