Laryngeal Cancer
Laryngeal cancer — also called voice box cancer — has a range of effective treatment options, including surgery, radiation, and chemotherapy, but success depends on the cancer’s stage, location in the larynx, and the patient’s overall health. For some patients, medical tourism can expand access to specialized teams and advanced technology at lower cost; if you consider care abroad, plan carefully to coordinate diagnosis, treatment and follow-up between your international team and local doctors.
Navigating Laryngeal Cancer: Advanced Treatment Options & Global Care for Your Voice and Health
A diagnosis of laryngeal cancer (voice box cancer) can be overwhelming. The larynx plays key roles in breathing, swallowing, and speaking, so concerns about health, quality of life, and voice function are natural. Understanding the disease, common symptoms, risk factors, and the full range of treatment options is an important first step toward informed decisions and better outcomes.
Some people consider medical tourism to access specialized care, advanced technology, or lower-cost treatment abroad. Common searches include “laryngeal cancer symptoms,” “what causes voice box cancer,” and “best treatment for laryngeal cancer.” This guide explains symptoms and causes, outlines treatment and recovery expectations, and compares treatment and cost considerations across international care options.
Early detection matters: persistent hoarseness, trouble swallowing, or a lump in the neck deserve timely evaluation — especially if symptoms last more than two to three weeks. Many causes are linked to lifestyle factors such as smoking and drinking alcohol, while HPV and environmental exposures can also play a role. Knowing the warning signs helps you seek diagnosis and start appropriate treatment sooner.
If you’re weighing international care, consider factors beyond cost — specialist expertise, the specific therapies available (surgery, radiation, chemotherapy, targeted therapy, immunotherapy), and how follow-up will be coordinated with your local doctor. Below is a roadmap of what this article covers to help you navigate treatment choices and medical tourism options for laryngeal cancer.
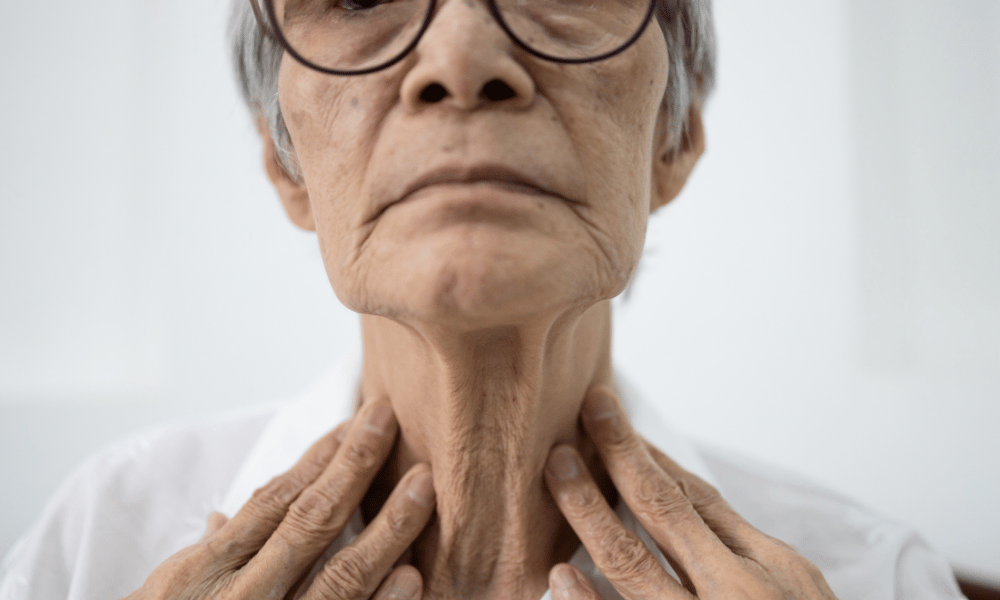
What are the Early Signs and Symptoms of Laryngeal Cancer?
Early signs of laryngeal cancer often involve changes in the voice (persistent hoarseness), throat discomfort, difficulty swallowing, or a lump in the neck. Any of these symptoms that do not improve should prompt timely medical evaluation.
Recognizing symptoms of laryngeal cancer early improves the chance of less extensive treatment and better functional outcomes. People commonly search for phrases like “hoarseness not going away” or “symptoms laryngeal cancer.” While many causes are benign, persistent signs—especially beyond two to three weeks—warrant an ENT consultation and appropriate tests.
- Persistent Hoarseness or Voice Changes: The most common early symptom, especially when the cancer affects the vocal cords; your voice may become raspy, weak, or intermittently lost. Singers and professional voice users should seek evaluation promptly for unexplained hoarseness.
- Persistent Sore Throat or Cough: A chronic sore throat or cough that doesn’t resolve with usual treatment can be a warning sign.
- Difficulty Swallowing (Dysphagia): Feeling that food gets stuck, or pain when swallowing, should prompt evaluation and tests to check the throat and esophagus.
- Ear Pain (Referred Pain): Pain felt in the ear on the same side as a throat problem can sometimes indicate a deeper issue in the larynx.
- Lump in the Neck: Swelling or a palpable lump may indicate enlarged lymph nodes from cancer spread and requires prompt assessment.
- Noisy or Difficult Breathing (Stridor): Occurs when a tumor narrows the airway — this is more common in advanced cases and is a medical urgency.
- Unexplained Weight Loss: Significant, unintentional weight loss can accompany many cancers, including laryngeal cancer.
When to see a doctor: if hoarseness, throat pain, or difficulty swallowing lasts more than two to three weeks, or if you notice a new neck lump or breathing problems, contact your doctor or an ENT specialist. Typical tests may include laryngoscopy, a biopsy, and imaging studies (CT, MRI, or PET) to determine the cause and stage of the disease.
What Causes Laryngeal Cancer and What are the Risk Factors?
The primary causes and risk factors for laryngeal cancer include prolonged tobacco use, heavy alcohol consumption, human papillomavirus (HPV) infection, and exposure to certain environmental or occupational toxins.
Knowing the main risk factors helps with prevention and earlier detection. People often search “what causes throat cancer” or “risk factors for voice box cancer.” While not everyone with these risk factors develops cancer, the following markedly increase the likelihood of developing laryngeal cancer:
- Tobacco Use: Smoking cigarettes, cigars, or pipes and using smokeless tobacco are the strongest modifiable risk factors. The chemicals in tobacco damage cells in the larynx over time and substantially raise risk.
- Alcohol (Drinking Alcohol): Heavy and long-term alcohol use increases laryngeal cancer risk, and the combination of alcohol plus tobacco multiplies that risk.
- Human Papillomavirus (HPV): Certain HPV types are linked to cancers of the throat. Evidence for HPV’s role in laryngeal cancer is growing but is stronger for oropharyngeal sites; discuss HPV testing with your doctor if relevant.
- Environmental and Occupational Exposures: Long-term exposure to substances such as wood dust, nickel, asbestos, and some industrial chemicals can increase risk in exposed workers.
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux can irritate the laryngeal lining over time and may contribute to risk in some people.
- Diet and Nutrition: Diets low in fruits and vegetables are associated with a modestly increased risk for head and neck cancers.
- Age and Gender: Laryngeal cancer is more common in older adults and historically has been more frequent in men, though patterns can vary by region and exposure.
How to reduce your risk: avoid tobacco, limit alcohol, maintain a healthy diet, manage reflux, and discuss HPV vaccination with your healthcare provider if you are eligible. If you have occupational exposures, follow workplace safety guidelines and report concerns to occupational health.
What are the Types of Laryngeal Cancer Treatments Available?
Treatment for laryngeal cancer depends on the tumor’s stage and exact location in the larynx. Common approaches include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy — often combined into an individualized treatment plan.
Choosing the right treatment involves weighing cancer stage, tumor site (glottic, supraglottic, subglottic), goals for voice preservation, and the patient’s overall health. Below are the main treatment options and when they are typically used.
- Surgery (When used: early to advanced, depending on location): Removal of the tumor is a core treatment. Options include:
- Endoscopic Surgery: Minimally invasive resection through the mouth for very early-stage tumors — often voice-sparing.
- Partial Laryngectomy: Removes only the cancerous part of the larynx to preserve some voice; appropriate for selected cases.
- Total Laryngectomy: Removes the entire larynx and creates a permanent stoma for breathing; used for extensive disease or when other options are not feasible. This requires speech rehabilitation.
- Neck Dissection: Surgical removal of lymph nodes when cancer has spread to the neck.
- Radiation Therapy (When used: early-stage as single therapy; combined with chemo for organ preservation): High-energy beams (including IMRT or proton therapy where available) precisely target cancer cells. Radiation can be definitive for early-stage glottic tumors or used after surgery to reduce recurrence risk.
- Chemotherapy (When used: advanced or metastatic disease; as part of chemoradiation): Systemic drugs (such as cisplatin-based regimens) are used to treat cancer cells throughout the body and are often combined with radiation to preserve the larynx in selected patients.
- Targeted Therapy (When used: tumors with specific molecular targets): Drugs that block particular molecules involved in tumor growth — these may have fewer systemic side effects than traditional chemotherapy and are chosen based on tumor markers.
- Immunotherapy (When used: recurrent or metastatic disease): Treatments that stimulate the immune system (e.g., checkpoint inhibitors) are an option for some advanced cases, especially when standard treatments have failed.
Trade-offs to discuss with your team: voice preservation versus complete tumor removal, potential side effects of radiation or chemotherapy, and rehabilitation needs after surgery. Treatment planning is best done by a multidisciplinary team — head and neck surgeons, radiation oncologists, medical oncologists, and speech therapists — who can tailor options to your stage and goals.
Who is Eligible for Laryngeal Cancer Treatment?
Eligibility for laryngeal cancer treatment is guided by the cancer’s stage and location, the patient’s overall health and prior therapies, and specific tumor features that help determine the safest and most effective treatment plan.
Deciding which laryngeal cancer treatments are appropriate is a team decision. Patients commonly ask, “Am I a candidate for surgery?” or “Can I have radiation instead?” A multidisciplinary team — including a head and neck surgeon, radiation oncologist, medical oncologist, and speech therapist — evaluates several key factors:
- Cancer Stage and Location: Early-stage disease (Stage I–II) may be treated with single-modality therapy (endoscopic surgery or radiation). Advanced stages (Stage III–IV) often need combined treatments (surgery plus radiation or chemoradiation). The tumor’s site within the larynx (glottic, supraglottic, subglottic) influences options and the likelihood of voice preservation.
- Overall Health and Performance Status: Medical conditions (heart, lung, kidney, liver disease) affect tolerance for surgery, radiation, or chemotherapy. Patients with better performance status are more likely to tolerate aggressive treatment.
- Tumor Biology and Pathology: Tumor grade, presence of HPV, and molecular markers can steer choices toward targeted therapy or immunotherapy in selected cases.
- Previous Treatments: Past surgery, radiation, or systemic therapy affects what can be offered next—recurrent disease requires a different strategy than newly diagnosed cancer.
- Patient Priorities and Preferences: Choices about voice preservation, acceptable side effects, and quality-of-life goals are central to shared decision-making.
Typical tests used to determine eligibility include laryngoscopy with biopsy, CT or MRI of the neck, and PET scan when indicated to assess cancer spread and lymph nodes. Questions to bring to your doctor: “Will this preserve my voice?”, “What are the main side effects?”, and “How will follow-up be coordinated?” A clear staging workup and honest discussion with your multidisciplinary team will define the best, individualized treatment plan.
What is the Recovery Time and Expectations After Laryngeal Cancer Treatment?
Recovery after laryngeal cancer treatment varies widely by the chosen therapy — from a few weeks after radiation to several months (or longer) after major surgery such as total laryngectomy — and typically requires focused rehabilitation for speech and swallowing.
Recovery is a process that depends on the treatment intensity, the patient’s overall health, and whether additional therapies (radiation or chemotherapy) are needed. Below are common expectations and a practical timeline to help you prepare.
- After Radiation Therapy:
- Short-term (weeks): Expect fatigue, sore throat, mucositis (mouth/throat soreness), skin redness, temporary voice changes, and some difficulty swallowing.
- Long-term (months+): Persistent dry mouth (xerostomia), taste changes, chronic voice alteration, and occasional swallowing problems; many symptoms improve gradually over months with supportive care.
- After Partial Laryngectomy (surgery):
- Hospital stay: Often a few days to a week, depending on recovery and swallowing function.
- Early home recovery (weeks): Hoarseness and swallowing difficulty are common; diet modifications and temporary feeding support may be needed.
- Full recovery: Many patients see substantial voice and swallowing improvement over 2–3 months with speech and swallowing therapy.
- After Total Laryngectomy (surgery):
- Hospital stay: Typically 1–2 weeks, longer if complications occur.
- Initial recovery: You will breathe through a permanent stoma in the neck, learn stoma care, manage secretions, and adapt to changes in smell and taste.
- Long-term rehabilitation: Speech rehabilitation (esophageal speech, tracheoesophageal puncture voice prosthesis, or electrolarynx), swallowing therapy, and psychological support are essential and may take many months; adaptation is often lifelong.
- After Chemotherapy / Targeted Therapy / Immunotherapy: Side effects vary by drug but commonly include fatigue, nausea, hair loss, low blood counts, and increased infection risk; most treatment-related side effects improve in weeks to months after therapy ends.
Rehabilitation is a cornerstone of recovery. Speech-language pathologists, dietitians, and occupational or physical therapists help restore communication and swallowing, manage nutrition, and improve quality of life. Practical tips: arrange follow-up with local providers before travel, pack necessary medical documents and medications, and plan for extra recovery time when considering treatment abroad.
Red flags — contact your doctor immediately if you experience: fever, increasing wound bleeding, sudden difficulty breathing, uncontrolled pain, or signs of infection. Early recognition of complications improves outcomes.
What are the Procedure Risks and Side Effects of Laryngeal Cancer Treatment?
Laryngeal cancer treatments can be effective but carry a range of risks and side effects that may affect voice, swallowing, breathing, and overall quality of life. Understanding common effects and how they are managed helps patients prepare and recover more smoothly.
Every treatment has potential side effects; some appear during or shortly after therapy (acute), while others can persist long-term. Below are the typical procedure-specific risks and practical notes on management you can discuss with your care team.
- Surgery (Laryngectomy):
- Voice loss: Total laryngectomy removes the natural voice source; voice rehabilitation (esophageal speech, tracheoesophageal puncture voice prosthesis, or an electrolarynx) can restore communication but requires training.
- Breathing changes: A permanent stoma (opening) in the neck changes breathing and requires stoma care to reduce infection and irritation.
- Swallowing and aspiration risk: Surgery can alter swallowing mechanics; swallowing therapy and diet adjustments help reduce aspiration risk.
- Surgical complications: Infection, bleeding, wound problems, and numbness in the neck/shoulder area can occur; most are treatable if identified early.
- Radiation Therapy:
- Acute side effects: Mucositis (sore, inflamed mouth/throat), skin redness, pain, difficulty swallowing, hoarseness, fatigue, and changes in taste are common during and shortly after radiation.
- Long-term effects: Dry mouth (xerostomia), dental problems, chronic voice changes, stiffness of neck muscles, lymphedema (neck swelling), and, rarely, osteoradionecrosis (jawbone damage). Many centers use advanced techniques (IMRT, proton therapy) to minimize exposure to healthy tissue.
- Management: Mouth rinses, pain control, swallowing exercises, dental care, saliva substitutes, and nutritional support help manage these effects.
- Chemotherapy:
- Common side effects: Nausea, vomiting, fatigue, hair loss, mouth sores, low blood counts (increasing infection risk), and neuropathy (nerve pain/tingling) can occur. Severity depends on the specific drugs and dose.
- Management: Antiemetics for nausea, growth factors for low blood counts, and dose adjustments or drug changes help reduce risks.
- Targeted Therapy and Immunotherapy:
- These agents often produce different side effects than chemotherapy. Targeted drugs may cause skin changes, diarrhea, or liver function abnormalities. Immunotherapy can trigger immune-related effects (rash, colitis, hepatitis, endocrinopathies) that require prompt recognition and sometimes immunosuppression.
- Management: Regular monitoring of labs and early reporting of symptoms to your doctor allows fast intervention and reduces serious complications.
Plain-language note: xerostomia means dry mouth that can make eating, speaking, and dental health harder; mucositis is painful sores inside the mouth or throat. Ask your team for specific plans to prevent and treat these conditions.
How these side effects are managed: supportive care (pain control, mouth care, nutritional support), rehabilitative services (speech and swallowing therapy), medications (anti-nausea, growth factors, steroids), and close follow-up. Always ask your doctor, “What side effects should I expect?” and “How will you manage them?” Early communication helps minimize long-term impact on voice and quality of life.
Worldwide Cost Comparison for Laryngeal Cancer Treatment
The cost of laryngeal cancer treatment varies widely by country, facility, and the exact mix of services included. While care in the USA and Western Europe can be substantially more expensive, medical tourism destinations often provide comparable medical expertise and technology at lower base prices — but total cost depends on many factors beyond the procedure itself.
Cost is a common reason patients consider medical tourism for laryngeal cancer. Searches such as “cost of laryngeal cancer surgery” or “affordable throat cancer treatment” reflect the financial burden many face. The table below offers estimated ranges to illustrate typical differences — treat these as ballpark figures that must be confirmed with specific hospitals and written quotes.
| Treatment ComponentUSA / Western Europe (Est.)Medical Tourism Destinations (e.g., India, Turkey, Mexico, Thailand) (Est.) | ||
| Total Laryngectomy (Surgery Only) | $30,000 – $70,000 | $10,000 – $25,000 |
| Partial Laryngectomy (Surgery Only) | $20,000 – $50,000 | $8,000 – $20,000 |
| Radiation Therapy (Full Course) | $20,000 – $60,000 | $7,000 – $18,000 |
| Chemotherapy (per cycle, varies) | $5,000 – $15,000 | $1,500 – $5,000 |
| Overall Treatment Plan (Combined therapies, complex cases) | $50,000 – $150,000+ | $15,000 – $45,000+ |
What these estimates include — and what they don’t: ranges above typically reflect procedural costs, basic hospital stay, and standard perioperative care. They may not include extra items such as international travel, accommodation, extended rehabilitation, prosthetic voice devices, specialized medications, or complex complications. When requesting a quote, ask for an itemized breakdown: surgeon fees, anesthesia, hospital room charges, imaging and pathology, rehabilitation, and post-discharge follow-up. A sample cost scenario to request: total laryngectomy + 4–6 weeks inpatient/outpatient rehab + two post-op follow-ups.
Why Consider Laryngeal Cancer Treatment Abroad?
Considering laryngeal cancer treatment abroad can offer meaningful cost savings and access to specialized expertise and advanced technology, but it’s important to weigh benefits against continuity of care and follow-up needs.
For some patients, medical tourism is a practical option when local care is limited, wait times are long, or the cost of care at home is prohibitive. Typical reasons people explore treatment abroad include lower procedural costs, access to experienced head and neck teams, and availability of specific technologies or clinical trials.
- Significant cost savings: As the cost comparison shows, treatment abroad can reduce out-of-pocket expenses — a key factor when financing a complex laryngeal cancer treatment plan.
- Access to specialized expertise and technology: Some international centers concentrate experience in head and neck cancer, offering specialized surgeons, multidisciplinary teams, and advanced options such as IMRT, proton therapy, or specialized reconstructive procedures.
- Potentially reduced wait times: In systems with long queues, traveling can shorten the time to definitive treatment — but this advantage depends on the destination and facility.
- Personalized and private care: Many medical tourists report more attentive, patient-centered service, with bundled support for logistics, language, and accommodation.
- Access to new approaches: Some centers offer clinical trials or novel therapies that may not be available or affordable at home — confirm trial eligibility and enrollment policies before planning travel.
Who should consider it: patients facing high local costs, those needing a specific specialist or technology not available locally, or patients willing to coordinate follow-up care with their home doctor. When it makes sense to stay local: if you require close, long-term follow-up that would be hard to arrange after travel, or if your condition is unstable and needs immediate local support.
Example scenario: a patient with an early-stage glottic tumor in a region with long surgical waitlists opts to travel to a specialist center for endoscopic voice-sparing surgery and returns home for follow-up rehabilitation with a local speech therapist — saving time and preserving voice. Always discuss plans with your local doctor and the overseas team to ensure seamless coordination of care.
Which Countries Offer the Best Value for Laryngeal Cancer Treatment?
Countries such as India, Turkey, Mexico, Thailand, South Korea, and Malaysia are frequently cited as top medical tourism destinations for laryngeal cancer because they combine experienced head and neck teams, modern facilities, and more competitive pricing than many Western centers.
When patients search for the “best countries for laryngeal cancer treatment” or “top hospitals for throat cancer abroad,” several nations consistently appear due to their balance of clinical expertise, international accreditation, and patient support services. Below are practical notes on each destination and how to choose between them.
- India: Known for highly skilled surgeons and large, specialized cancer centers (many JCI-accredited). India often offers complex head and neck surgery and comprehensive rehabilitation at comparatively low cost.
- Turkey: A growing hub for medical tourism with modern hospitals in Istanbul and Ankara, experienced ENT and oncology teams, and competitively priced treatment for European and Middle Eastern patients.
- Mexico: Popular with North American patients due to proximity and lower travel costs; major cities and border hospitals provide accessible oncology services and shorter travel times.
- Thailand: Recognized for combining high-quality clinical care with strong patient services and hospitality; Bangkok hosts several internationally accredited cancer centers.
- South Korea: Excelling in advanced technology and innovative therapies, South Korea can be a top choice when cutting-edge diagnostics or reconstructive expertise are priorities, though costs can be higher than other Asian destinations.
- Malaysia: Offers affordable, quality care with English-speaking staff and several JCI-accredited hospitals, making coordination and communication easier for international patients.
How to choose between countries: consider visa requirements and ease of travel, language and interpreter availability, the hospital’s accreditation (look for JCI or recognized national bodies), documented surgeon experience in head and neck cancer, availability of the specific treatment you need (e.g., IMRT, proton therapy, complex reconstruction), and plans for post-treatment follow-up at home.
Red flags to avoid: hospitals without accreditation or outcome data, vague cost estimates, lack of a clear post-treatment follow-up plan, or providers unwilling to communicate directly with your local doctor. Always verify credentials, ask for outcome statistics for similar cases, and confirm what services are included in any quoted price.
What to Expect When Traveling for Laryngeal Cancer Treatment Abroad?
Expect coordinated support when traveling for laryngeal cancer care: many hospitals and facilitators help with treatment planning, travel logistics, language support, and arrangements that span initial consultation through post-operative follow-up.
Traveling for treatment requires careful preparation. While many medical tourism providers streamline the process, it’s important to know what is typically included, what you must arrange, and how to keep your local doctor involved. Below is a practical outline of the usual steps and a brief pre-travel checklist.
- Initial consultation and case review: You’ll normally submit medical records (pathology reports, imaging, operative notes) for review. The international team or facilitator provides a proposed treatment plan, timeline, and an estimated, itemized cost.
- Travel logistics and accommodation: Many facilitators assist with visa guidance, flight bookings, airport transfers, and hotel arrangements; confirm which services are included and the fees for any extras.
- Language support: Reputable hospitals typically offer interpreters or multilingual staff—verify availability for all stages of care (consultation, consent, and post-op instructions).
- Pre-treatment evaluation: On arrival you may undergo repeat or additional tests (endoscopy, CT/MRI, labs) to confirm the plan. Allow time in your schedule for this repeat workup.
- Treatment and hospital stay: The facility will deliver your chosen therapy (surgery, radiation, or systemic treatment) and provide inpatient care as needed; ask for a clear timeline for hospital discharge and rehabilitation.
- Post-treatment follow-up: Before you return home, secure written post-op care instructions, rehabilitation plans (speech/swallowing therapy), and a schedule for remote follow-up. Confirm how urgent issues will be handled once you’re back home.
- Recuperation and light tourism: If your medical team approves, light rest or sightseeing is sometimes possible during recovery—plan conservatively and prioritize health.
Pre-travel checklist: bring complete medical records (digital and printed), current medication list, contact details for your home doctor, travel insurance that covers your treatment, passport/visa documents, and a plan for local follow-up care after you return.
What may not be included in initial quotes: long-term rehabilitation, prosthetic voice devices, extended hospital stays for complications, local medications after discharge, and domestic follow-up visits—always request an itemized quote and confirm who is responsible for post-discharge care. To vet a facilitator or hospital, ask for accreditation information, surgeon experience with head and neck cancer, patient references, and a sample itinerary with timelines and costs.
How to Ensure Safety and Quality for Laryngeal Cancer Treatment Abroad?
To safeguard safety and quality when seeking laryngeal cancer care overseas, prioritize accredited hospitals, verify surgeon and team credentials, review outcomes and patient feedback, obtain a detailed cost breakdown, and confirm a clear post-treatment follow-up plan.
Choosing an overseas provider requires careful vetting. Below are practical steps, sample questions to ask, and red flags to watch for when evaluating hospitals, doctors, and facilitators for laryngeal cancer care.
- Choose accredited hospitals: Look for international accreditation such as JCI and recognized national accreditations. Accreditation indicates that a hospital follows international quality and patient safety standards.
- Verify physician credentials: Ask for the treating surgeon’s and oncologist’s qualifications, board certifications, and specific experience with head and neck and laryngeal cancer procedures. Sample question: “How many laryngectomies or voice-preserving surgeries have you performed in the past year?”
- Request outcome data and patient references: Seek case volumes, complication rates, and (if available) survival or functional outcomes for similar cases. Patient testimonials can help but ask for clinical outcome metrics where possible.
- Get a detailed, itemized quote: Ensure the quote covers diagnostics, surgeon and hospital fees, anesthesia, prosthetic devices (if needed), rehabilitation, and follow-up. Clarify which costs are excluded (travel, accommodation, long-term rehab).
- Confirm communication and language support: Verify interpreter availability and direct communication channels between you, the overseas doctor, and your home physician for coordinated care.
- Vet facilitators carefully: If using a medical tourism facilitator, ask how they vet hospitals and doctors, request references, and confirm whether they handle logistics only or also clinical coordination. Ask specifically about their experience arranging head and neck cancer cases.
- Confirm post-treatment follow-up: Make sure there is a written plan for follow-up visits, wound care, rehabilitation (speech and swallowing), and remote consults after you return home.
Red flags: lack of accreditation or outcome data, vague pricing, no clear post-discharge plan, unwillingness to provide surgeon-specific experience, or poor communication. These should prompt caution and further verification.
In short, prioritize accredited hospitals (JCI and recognized national bodies), verified doctors with documented head and neck experience, transparent costs, and a written plan for follow-up care. Diligent research and clear communication are the best defenses for safety when pursuing laryngeal cancer treatment abroad.
What are Patient Success Stories from Abroad for Laryngeal Cancer?
Many international patients report positive outcomes after traveling for laryngeal cancer treatment, citing access to experienced head and neck teams, advanced therapies, and comprehensive rehabilitation that help restore voice function and improve quality of life.
Individual patient stories are confidential, so the evidence here is descriptive rather than a formal outcome comparison. Still, common themes emerge from medical tourists who sought treatment abroad for laryngeal cancer: timely access to specialized care, successful tumor control, and meaningful rehabilitation of speech and swallowing. If you consider traveling for care, ask providers for anonymized case examples and documented outcome metrics for similar cases.
Typical positive outcomes reported by patients include:
- Restored voice and swallowing: Patients undergoing partial laryngectomy or advanced speech rehabilitation after total laryngectomy often report improved communication and safer swallowing following structured rehab with speech-language pathologists.
- Access to innovative techniques: Receiving precision radiation (IMRT or, where available, proton therapy), minimally invasive endoscopic surgery, or specialized reconstructive procedures can contribute to better functional preservation when indicated.
- Expert surgical outcomes: High-volume head and neck surgeons in accredited centers may achieve effective tumor removal while maximizing functional preservation.
- Comprehensive rehabilitation: Coordinated programs that include speech-language pathology, dietitians, and psychological support often lead to more holistic recovery and better long-term quality of life.
- Empowerment through choice: Many patients feel empowered by being able to choose a center or treatment that aligns with their priorities—whether that is voice preservation, reduced wait times, or lower overall cost.
- High-quality care at a lower cost: A recurring benefit reported is receiving care that meets international standards without the higher price tag at home, easing financial stress for many families.
Realistic expectations: while many patients experience functional and emotional improvements, outcomes vary by stage, tumor biology, and individual health. Avoid assumptions that overseas care will guarantee better survival—ask for documented outcomes and discuss comparative data with your doctor.
Take the Next Step with DGS Healthcare
Ready to explore treatment laryngeal cancer options abroad? To get an accurate, itemized quote you’ll typically need to provide your medical records, pathology reports, and imaging scans. DGS Healthcare can help you discover top clinics, compare prices, and request a tailored quote.
Patient privacy note: individual stories are anonymized; ask any provider for de-identified case outcomes and published metrics for similar laryngeal cancer cases before you decide.
