Stereotactic Radiotherapy Treatment
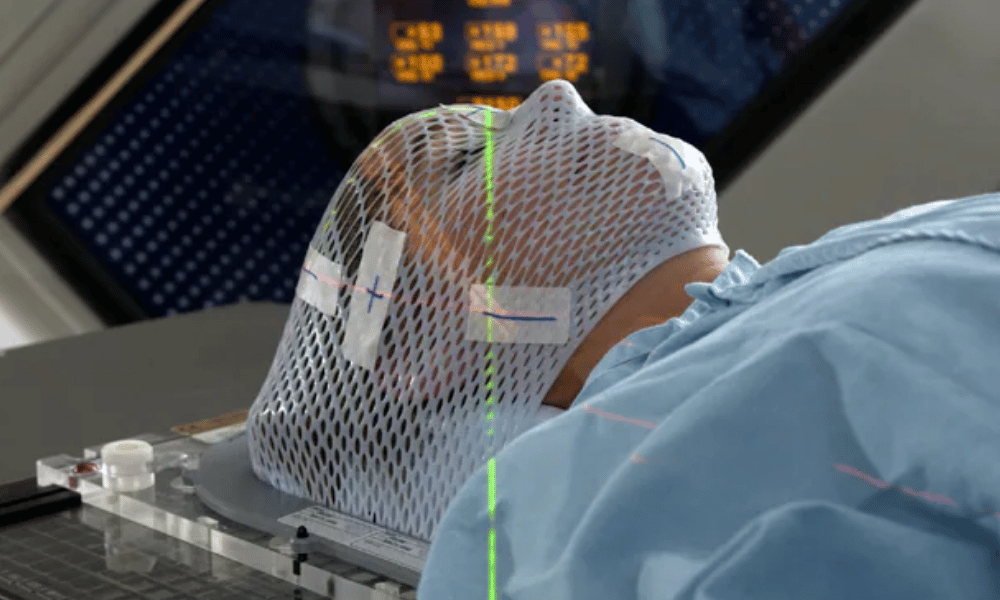
Stereotactic Radiotherapy (SRT) is a highly precise, non‑invasive radiation treatment that delivers focused, high doses to a defined target in fewer sessions, reducing exposure to surrounding healthy tissue. It’s commonly used for small tumors in the brain (stereotactic radiosurgery, SRS) and for lesions elsewhere in the body (stereotactic body radiotherapy, SBRT), often as an outpatient procedure.
Unlocking Precision: Your Guide to Stereotactic Radiotherapy for Advanced Cancer Care
Facing a cancer diagnosis can be overwhelming. When precision, minimal invasiveness, and shorter treatment courses matter, Stereotactic Radiotherapy (SRT) is a focused form of radiation therapy that delivers high, concentrated doses to a defined target, typically over one to five visits, while minimizing dose to surrounding healthy tissue.
SRT includes two main approaches: stereotactic radiosurgery (SRS) for brain and spine lesions—usually a single high‑dose session—and stereotactic body radiotherapy (SBRT) for tumors elsewhere in the body (for example, lung, liver, or prostate), typically delivered in a small number of fractions. Compared with conventional radiotherapy, SRT uses advanced imaging, precise planning, and motion management to concentrate the dose on the tumor and spare nearby organs.
SRT may be an option for patients with small to medium‑sized primary tumors, selected metastatic lesions, or when surgery is not feasible. Talk with your oncology team to learn whether stereotactic radiotherapy is appropriate for your specific condition; this guide explains how SRT works, who may benefit, what to expect, and considerations if you are exploring treatment abroad.
What symptoms might suggest Stereotactic Radiotherapy is needed?
Symptoms that prompt investigation are those caused by the underlying tumor or lesion — for example, headaches or seizures with a brain lesion, or persistent cough with a lung lesion. SRT is a treatment option once imaging confirms a treatable target, not a direct therapy for symptoms themselves.
If you have new, persistent, or worsening symptoms, see a healthcare professional. Symptoms alone do not confirm cancer; diagnosis typically requires imaging (MRI, CT, PET) and sometimes biopsy to identify a lesion that may be suitable for stereotactic radiosurgery or SBRT.
- Brain lesions (SRS): Persistent or progressive headaches, new seizures, changes in vision or hearing, new weakness or numbness on one side, balance or coordination problems, personality changes, nausea or vomiting.
- Lung lesions (SBRT): A cough that won’t go away or gets worse, new shortness of breath or wheeze, chest pain, unexplained weight loss or fatigue, hoarseness, or recurrent chest infections — all warrant evaluation for possible lung tumors including early-stage lung cancer.
- Prostate lesions (SBRT): Urinary frequency (especially at night), weak or interrupted urine flow, blood in urine or semen, pelvic or back pain, or painful ejaculation may prompt prostate evaluation.
- Liver lesions (SBRT): Unexplained weight loss, loss of appetite, nausea, abdominal pain or swelling, jaundice (yellowing of skin/eyes), or pale stools.
Example: if imaging shows a solitary 1–3 cm lung tumor in a patient who cannot or prefers not to have surgery, SBRT is commonly considered — but candidacy depends on location, nearby organs, and overall health. Always review findings and treatment options with your multidisciplinary team before deciding on SRT.
What causes or risk factors lead to conditions treated by Stereotactic Radiotherapy?
The causes and risk factors vary by the specific cancer or lesion that SRT treats—examples include smoking for lung cancer and chronic viral hepatitis for liver cancer. Remember: SRT is a targeted treatment for tumors; it does not prevent the underlying causes that led to the disease.
Stereotactic Radiotherapy is used to treat tumors that arise from a range of causes. Understanding common risk factors for those cancers supports prevention and early detection, which can improve treatment options and outcomes.
- Brain tumors: Many primary brain tumors have no clear cause, though prior therapeutic radiation and certain inherited syndromes (e.g., neurofibromatosis, Li‑Fraumeni) increase risk. Metastatic brain tumors arise when cancer spreads from other organs (commonly lung, breast, melanoma, kidney, colon).
- Lung cancer: Tobacco smoking is the leading risk factor; secondhand smoke, radon, asbestos and occupational carcinogens, prior chest radiation, and family history also raise risk.
- Prostate cancer: Risk increases with age (most cases after age 50), family history, and certain racial/ethnic factors; lifestyle and obesity may contribute to risk and outcomes.
- Liver cancer: Chronic hepatitis B or C infection, cirrhosis (from alcohol or metabolic disease), nonalcoholic fatty liver disease, and exposure to aflatoxins are common risk factors.
While SRT addresses the tumor itself with precise radiotherapy, prevention (smoking cessation, vaccinations for hepatitis B, screening where appropriate) and early diagnosis remain essential. For accuracy, consider citing authoritative sources such as the American Cancer Society or WHO when adding specific epidemiology or risk statistics.
What types of Stereotactic Radiotherapy treatments are available?
The main approaches are stereotactic radiosurgery (SRS) for lesions in the brain and spine, and stereotactic body radiotherapy (SBRT) for tumors elsewhere in the body (for example, lung, liver, or prostate). Both are forms of stereotactic radiotherapy that deliver precisely shaped, high doses of radiation over a small number of sessions to maximize tumor control while sparing healthy tissue.
SRT is an umbrella term for highly focused radiotherapy. Which technique is chosen depends on the tumor location, size, and surrounding anatomy:
- Stereotactic Radiosurgery (SRS):
- Primarily used for targets in the brain or spine. Despite the name, SRS is non‑surgical (no incision).
- Typically delivered in a single high‑dose session for small lesions; larger or complex targets may be treated with fractionated SRS (2–5 sessions).
- Common platforms: Gamma Knife (cobalt‑60 based system optimized for intracranial spherical targets), CyberKnife (robotic LINAC offering flexible beam angles for irregular shapes), and LINAC‑based systems equipped for SRS.
- Stereotactic Body Radiotherapy (SBRT):
- Used for tumors outside the brain and spine (lungs, liver, prostate, kidney, pancreas, bone).
- Delivers high doses per fraction over a few treatment sessions (commonly 1–5 fractions, though schedules vary by site and proximity to critical structures).
- SBRT requires motion management (breath‑hold, gating, tracking) and advanced imaging during planning and delivery to ensure the dose accurately covers the moving tumor while protecting nearby organs.
- Typically delivered with modern LINAC platforms (including systems marketed for SBRT) or robotic systems like CyberKnife.
In short, SRS is optimized for intracranial/spinal targets and often uses a single session, while SBRT is adapted for body sites and uses motion‑aware planning across a few fractions. Both prioritize delivering an effective dose to the tumor while minimizing exposure to surrounding healthy tissue through precise planning and image‑guided delivery.
Who is eligible for Stereotactic Radiotherapy, and how is candidacy determined?
Eligibility for SRT depends on tumor size, location, type, number of lesions, prior treatments, and the patient’s overall health. A multidisciplinary team reviews imaging, pathology, and medical history to create a personalized radiotherapy plan.
Determining candidacy for stereotactic radiotherapy is a careful, case-by-case process. Below are the primary factors your team will consider and a short “typical workup” checklist so you know what to expect.
- Tumor characteristics:
- Size: SRT is usually best for small to medium lesions (many centers consider tumors under ~5 cm more suitable), though exceptions exist depending on location and technique.
- Location: Proximity to critical structures (nerves, major vessels, spinal cord) affects planning and allowable dose; tumors “located near” sensitive tissues may need modified fractionation or alternative approaches.
- Number and type: SRT is commonly used for one to a few lesions (oligometastases) and for select primary tumors or benign lesions depending on biology and goals of care.
- Patient health and prior treatments:
- Performance status and co‑morbidities: Patients need sufficient fitness to undergo planning and treatment visits; existing conditions are reviewed to avoid complications.
- Prior radiation: If prior radiotherapy was given to the same area, accumulated dose to healthy tissue may limit SRT or require tailored planning.
- Multidisciplinary assessment and planning:
- A team typically includes radiation oncologists, medical physicists, neurosurgeons (for brain/spine), medical oncologists, and nurse coordinators to balance efficacy and safety.
- Planning: High‑quality imaging (MRI, CT, PET), careful contours, dose calculations, and motion management are essential to protect healthy tissue while delivering the therapeutic dose.
Typical workup checklist:
- Relevant imaging (MRI/CT/PET) and any available pathology reports.
- Review of prior treatments and radiation records (if applicable).
- Assessment of performance status and co‑morbidities.
- Multidisciplinary discussion and a documented treatment plan with dose, fractionation, and follow‑up schedule.
Your radiation oncologist will explain whether SRT is the preferred treatment, what dose and fractionation are planned, and how the team will minimize risks. If you are considering treatment abroad, confirm the team composition and planning process to ensure continuity of care.
What can I expect during recovery after Stereotactic Radiotherapy?
Recovery after SRT is usually quick because the procedure is non‑invasive and highly targeted. Many patients resume normal activities within a day or two, although some temporary side effects such as mild fatigue or local irritation are possible.
Because stereotactic radiotherapy is typically delivered as an outpatient treatment, downtime is limited. Expect individualized recommendations from your team based on the treatment area and dose plan.
- Immediate post‑treatment:
- Most patients go home the same day; rare exceptions include those who require monitoring after sedation or with significant co‑morbidities.
- Mild fatigue is common and often resolves within hours to days.
- If a head frame was used for SRS, expect minor soreness at pin sites that can be managed with over‑the‑counter analgesics.
- Days to weeks after treatment:
- Low downtime: Many patients return to light work and normal daily activities within a day or two; heavier exertion should follow your team’s guidance.
- Common short‑term side effects: fatigue (most frequent), and localized symptoms depending on site — e.g., headache or nausea after brain SRS; mild cough or chest wall discomfort after lung SBRT; temporary urinary urgency after prostate SBRT; mild abdominal discomfort after liver SBRT.
- Practical tips: stay hydrated, rest as needed, avoid heavy lifting for a few days unless directed otherwise, and keep a log of new or worsening symptoms to report to your team.
- Long‑term expectations and follow‑up:
- The goal of SRT is durable tumor control; follow‑up visits and imaging (timing varies by center but often occur within 6–12 weeks and periodically thereafter) monitor response and late effects.
- Report any persistent or new symptoms promptly — severe shortness of breath, high fever, sudden neurological changes (weakness, speech or vision changes), or uncontrolled vomiting warrant urgent contact.
Recovery timelines vary with the treated area, total dose, and individual factors. Your radiation oncologist will give specific guidance about expected side effects, follow‑up imaging, and when it’s safe to resume normal activities. If you are receiving treatment abroad, confirm follow‑up plans and how your home team will continue care.
What are the potential risks and side effects of Stereotactic Radiotherapy?
Although SRT delivers radiation with high precision, it still carries potential risks such as temporary swelling (edema), fatigue, and localized irritation. The likelihood and type of side effects depend on the treated area, the planned dose radiation, and individual patient factors.
Stereotactic radiotherapy aims to maximize dose to the tumor while reducing exposure to healthy tissue, but no treatment is without effects. Below are common, less common, and organ‑specific side effects to discuss with your team.
Common, usually temporary side effects
- Fatigue: The most frequent complaint after radiotherapy; usually mild to moderate and transient.
- Nausea: May occur when treating the head or upper abdomen but is often controllable with medication.
- Headaches: Possible after brain SRS, often related to temporary swelling and manageable with steroids or analgesics if needed.
- Skin irritation: Mild redness or dryness at the treatment area is less common than with conventional radiotherapy but can occur.
- Local discomfort: Site‑specific tenderness (e.g., chest wall soreness after lung SBRT or urinary changes after prostate SBRT).
Less common or more serious risks
- Swelling (edema): Radiation can cause temporary swelling around treated brain tissue; steroids are commonly used to control symptoms.
- Radiation necrosis: Rarely, irradiated tissue can undergo necrosis, causing persistent swelling or new symptoms; management may include steroids, medical therapies, or surgery in select cases.
- Nerve or organ damage: When tumors are close to critical nerves or organs there is a small risk of lasting deficits (weakness, numbness, or organ dysfunction), which careful planning and dose constraints aim to avoid.
- Organ‑specific concerns:
- Lung SBRT: Risk of radiation pneumonitis or fibrosis (can cause persistent cough or shortness of breath).
- Liver SBRT: Rare risk of radiation‑induced liver injury; careful dose planning reduces this risk.
- Prostate SBRT: Possible temporary or, rarely, chronic urinary or bowel changes (urgency, bleeding).
- Hair loss: Localized hair loss may occur if scalp is in the radiation path for brain targets; this may be temporary or, less commonly, permanent.
When to call your doctor
- Signs of infection or high fever, severe or worsening shortness of breath, new or worsening neurological deficits (sudden weakness, slurred speech, vision changes), uncontrolled vomiting, or severe pain.
Risk profiles depend on planned doses and cumulative doses if prior radiotherapy was given; your radiation oncologist and physics team will review dose constraints and expected risk side effects during planning. Ask your team for approximate likelihoods based on published data for your specific treatment area if you want numerical risk estimates.
How does the cost of Stereotactic Radiotherapy compare worldwide?
The cost of SRT varies widely by country, facility, treatment type (SRS vs SBRT), the number of fractions, the treated body part, and the technology used. In many medical‑tourism destinations, comparable quality care can be available at substantially lower prices than in the United States.
When comparing costs, note that prices often reflect the procedure itself and may or may not include pre‑treatment planning, imaging, pathology, travel, accommodation, or post‑treatment follow‑up. Exact pricing depends on the clinic’s package, the complexity of planning, and the number of sessions required.
Stereotactic Radiotherapy Cost Comparison (Estimated Ranges in USD)
| Region/CountryEstimated Cost Range (per treatment course)Typical Savings Compared to US | ||
| United States | $20,000 – $70,000+ | (Base for comparison) |
| Western Europe (e.g., UK, Germany) | $15,000 – $45,000 | 20% – 40% |
| India | $5,000 – $15,000 | 70% – 90% |
| Thailand | $8,000 – $20,000 | 60% – 85% |
| South Korea | $10,000 – $25,000 | 50% – 75% |
| Turkey | $7,000 – $18,000 | 65% – 85% |
| Mexico | $8,000 – $22,000 | 60% – 80% |
*These are estimated ranges (approximate) and can vary by hospital, city, and individual patient needs. Confirm what is included in any quote—planning, imaging, pathology, follow‑up, travel, and accommodation may be itemized separately.
If you are considering treatment abroad, compare itemized quotes, verify accreditations and technology, ask about the expected number of treatment days and overall timeline, and confirm how follow‑up care will be coordinated with your local team or the treating center.
Why should I consider Stereotactic Radiotherapy abroad for my treatment?
Seeking SRT abroad can offer meaningful advantages for some patients, including lower overall costs, faster access to specialized care, and access to advanced technology and experienced teams — but choices should be made after careful vetting and planning for continuity of care.
Traveling for stereotactic radiotherapy is a personal decision. For many, it is attractive because it can combine high‑quality treatment with better value or timelier access. Below are practical reasons patients consider treatment abroad and the questions to ask when comparing options.
- Cost savings: Even after adding travel and accommodation, total costs for SRT (SRS or SBRT) can be substantially lower in many international centers compared with some Western countries, making treatment more accessible for patients with limited coverage.
- Access and timing: Some patients experience shorter wait times abroad for specialized radiotherapy appointments and planning — important when timely treatment affects outcomes.
- Technology and expertise: Many international centers invest in state‑of‑the‑art platforms (Gamma Knife, CyberKnife, advanced LINACs) and have multidisciplinary teams experienced in stereotactic body radiation and intracranial radiosurgery.
- Personalized care and logistics support: Clinics that serve international patients often provide coordinated packages, international patient coordinators, language services, and help with travel arrangements.
- Privacy and environment: Some patients prefer the privacy and restorative environment of receiving care away from home.
Before deciding, ask direct questions to compare clinics and teams: What are the physicians’ credentials and annual SRT case volumes? Which specific equipment and planning systems are used? What is included in the quoted price (planning, imaging, follow‑up)? How is follow‑up care coordinated with your local oncology team? What are contingency plans for complications? Verifying accreditation, clinician experience, and clear communication channels helps ensure safe, effective treatment abroad.
Which countries offer the best value and quality for Stereotactic Radiotherapy?
Several countries are frequently chosen by international patients for the combination of value, advanced technology, and experienced teams for stereotactic radiotherapy. Individual hospitals vary, so evaluate centers by accreditation, clinician credentials, and the specific equipment they use.
When considering SRT abroad, look for verifiable quality markers (JCI or national accreditation), physicians’ SRT case volume, published outcomes where available, and the presence of modern planning and delivery systems (e.g., Gamma Knife, CyberKnife, TrueBeam). The countries below are commonly cited for offering strong value and quality.
- India:
- Value: One of the most affordable destinations for SRT.
- Quality: Numerous JCI‑accredited hospitals and centers with experienced radiation oncology teams and modern LINAC/CyberKnife/Gamma Knife platforms; many centers serve international patients.
- Thailand:
- Value: Competitive pricing with high service levels.
- Quality: Many private hospitals offer comprehensive international patient services and advanced SBRT/SRS technology; English language support is common.
- South Korea:
- Value: Moderately priced with excellent outcomes.
- Quality: Leading technology and strong research focus; many centers have state‑of‑the‑art radiotherapy platforms and multidisciplinary teams.
- Turkey:
- Value: Competitive pricing for advanced procedures.
- Quality: Rapidly growing medical tourism sector with many accredited hospitals offering modern radiotherapy services.
- Mexico:
- Value: Convenient and cost‑effective option for North American patients.
- Quality: Major centers in border cities and large urban areas often have experienced teams and modern equipment, sometimes with US‑trained specialists.
- Germany:
- Value: Generally higher costs than some Asian destinations but often still competitive with the US for select services.
- Quality: Renowned for rigorous clinical standards, advanced research, and high‑quality facilities—an option for patients prioritizing top clinical standards.
Note: not every hospital in these countries meets the same standards—always verify accreditation (JCI or equivalent), confirm which specific radiotherapy platforms are available (e.g., Gamma Knife, CyberKnife, Varian TrueBeam), review physician credentials and patient outcomes where possible, and read verified patient reviews before making decisions.
How can I ensure safety and quality when seeking Stereotactic Radiotherapy abroad?
To maximize safety and quality when pursuing SRT abroad, prioritize internationally accredited hospitals, verify physician and team credentials, confirm the specific technology and quality‑assurance protocols used in planning and delivery, and ensure clear communication and post‑treatment continuity of care.
Choosing a center for stereotactic radiotherapy (SRS or SBRT) requires due diligence. Use the checklist below to evaluate clinics, request documentation, and plan for follow‑up care with your local team.
- Check accreditation and facility standards:
- Look for JCI or equivalent accreditation and evidence of the center’s radiation safety and QA programs (Joint Commission International (JCI)).
- Verify physician credentials and team experience:
- Ask for the radiation oncologist’s board certifications, SRT specialization, and annual case volumes. Request experience details for medical physicists and neurosurgeons (if applicable).
- Confirm technology and planning protocols:
- Verify which platforms are used (e.g., Gamma Knife, CyberKnife, Varian TrueBeam, Elekta Versa) and request information on imaging capabilities, motion management, and planning systems.
- Ask about quality assurance records, machine calibration schedules, and typical planning time (how many minutes/hours between scans and planned treatment sessions).
- Request documentation and outcome information:
- Request sample treatment plans, complication rates or published outcomes if available, physician case volumes, and QA certification documents.
- Ensure clear communication and record sharing:
- Arrange language support if needed, and have all imaging and pathology translated and sent in advance. Confirm how plans and reports will be shared with your local oncologists for continuity of care.
- Use reputable facilitators carefully:
- If you use a medical tourism service (for example, PlacidWay), verify the facilitator’s vetting process and confirm direct access to clinicians for clinical questions rather than only administrative contacts.
- Understand the full treatment and follow‑up plan:
- Obtain a written plan detailing pre‑treatment evaluations, dose and fractionation, expected number of clinic visits and minutes per positioning/session, post‑treatment imaging schedule (scans), and contingency plans for complications or unexpected findings.
By following this checklist—verifying radiotherapy accreditation, clinician experience, planning processes, and follow‑up arrangements—you can significantly reduce risk and improve the chance of a successful outcome. Always coordinate plans with your home oncology team so care is continuous and well‑documented.
Take the Next Step with DGS Healthcare
Ready to explore stereotactic radiotherapy treatment options abroad? Compare accredited clinics, review physician credentials and technology, and get a free, personalized quote from DGS Healthcare.
Have your imaging reports and pathology available for the fastest, most accurate quote. Typical response time: 24–72 hours.
