Adrenal Gland Cancer Treatment
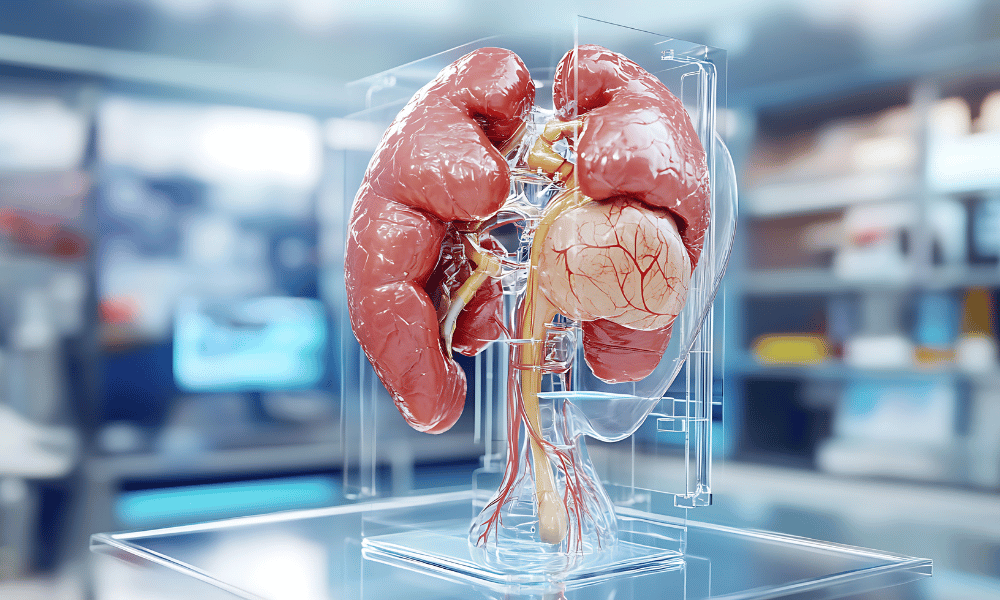
Adrenal Gland cancer affects the small adrenal glands that sit above each kidney; treatment usually involves diagnosing and removing the tumor (adrenalectomy) and may include radiation or chemotherapy. Many patients explore international treatment options for access to specialized centers and potential cost savings. Early detection and expert, timely care improve outcomes.
Navigating Adrenal Gland Cancer: Your Guide to International Treatment Options
A diagnosis of adrenal gland cancer can be overwhelming. These small endocrine organs, located atop the kidneys, make hormones that regulate blood pressure, metabolism, stress response, and more; when abnormal cells grow there they can disrupt that balance and require specialized care. Many patients consider all available options — including seeking treatment abroad — to access experienced teams and advanced care.
Adrenal tumors include several distinct conditions: adrenocortical carcinoma (ACC) arises from the adrenal cortex and can produce excess cortisol, aldosterone, or sex hormones; pheochromocytoma (from the adrenal medulla) and related paragangliomas produce adrenaline-type hormones and have different risks and preparations for surgery. ACC is rare compared with benign adrenal masses, but all merit careful evaluation.
This guide covers causes, symptoms, diagnostic tests, common treatments (from adrenalectomy to mitotane, radiation, and targeted therapies), recovery expectations, and how to evaluate international treatment options safely. Quick roadmap: symptoms & diagnosis → causes & risk → treatments & recovery → costs & choosing a destination.
We aim to provide clear, evidence-informed, and empathetic information so you can discuss next steps with your endocrine and oncology team. If you have new or concerning symptoms, contact your doctor promptly — and consider collecting your medical records and imaging if you plan to seek an international second opinion.
What are the common symptoms and warning signs of adrenal gland cancer?
Symptoms can be subtle and depend on whether the tumor is functioning (producing hormones) or non‑functioning; common clues include hormone-related changes such as new high blood pressure or unexplained weight shifts, or local symptoms from a growing mass.
Adrenal tumors may produce excess hormones (cortisol, aldosterone, androgens, or adrenaline-type hormones) or cause symptoms by pressing on nearby structures. Below are the typical symptom groups — presented as short, scannable points — and a quick guide on when to see a doctor.
- Hormone-related symptoms (functioning tumors):
- Excess cortisol (Cushing’s-like): Central weight gain (face, neck, trunk), muscle weakness, easy bruising, purple stretch marks, mood changes, new or worsening diabetes.
- Excess aldosterone (Conn’s-like): Persistent high blood pressure, low potassium (may cause muscle cramps), fatigue, frequent urination.
- Sex steroid excess (androgens/estrogens): Women: increased facial/body hair, voice deepening, male-pattern hair loss. Men: breast enlargement, low libido. Children: early or abnormal puberty.
- Tumor-pressure symptoms:
- Abdominal or flank pain, a palpable mass, feeling of fullness or bloating, unexplained weight loss, or new back pain — especially if persistent or progressive.
- Pheochromocytoma / medulla-related symptoms: Paroxysms of very high blood pressure, rapid heart rate, sweating, headaches, tremor, anxiety or panic-like episodes. These are episodic and can be mistaken for panic attacks.
How common are functioning tumors? A minority of adrenal masses produce hormones; among malignant adrenal tumors (like adrenocortical carcinoma), a notable portion are functioning — exact percentages vary by series, so discuss your case with an endocrinologist.
When to see a doctor: New, persistent, or worsening symptoms — especially new high blood pressure, unexplained weight gain or loss, new facial/body hair changes, episodic high blood pressure with sweating/heart palpitations, or persistent abdominal/back pain — warrant medical evaluation and diagnostic tests (blood tests, hormone panels, and imaging scans).
What causes adrenal gland cancer, and who is at higher risk?
The precise cause of most adrenal gland cancers is unknown, but many arise from genetic mutations in adrenal cells. While some cases are linked to inherited syndromes, the majority are sporadic—occurring in people without a clear family history.
Adrenal cancers typically result from DNA changes in adrenal gland cells that lead to uncontrolled growth. Patients commonly search for “adrenal tumor causes” or “who is at risk.” Below are the established risk factors and genetic associations to discuss with your care team and genetic counselor.
- Inherited genetic syndromes: A subset of adrenal cancers—especially adrenocortical carcinoma (ACC) in children and young adults—are linked to inherited conditions. Consider genetic counseling if you have a family history or early-age diagnosis. Examples include:
- Li‑Fraumeni syndrome (TP53 mutation): Autosomal dominant; raises risk of ACC and other cancers.
- Beckwith‑Wiedemann syndrome: An overgrowth syndrome seen in children that increases pediatric cancer risk, including ACC.
- Multiple Endocrine Neoplasia type 1 (MEN1): Can be associated with endocrine tumors, sometimes affecting the adrenal glands.
- Familial Adenomatous Polyposis (FAP): Primarily a colorectal cancer syndrome but occasionally linked to adrenal tumors.
- Carney complex: A rare syndrome that increases the risk of various endocrine and nonendocrine tumors, including adrenal lesions.
- Sporadic (non‑inherited) cases: Most adrenal cancers occur without a known family history and are thought to arise from random mutations that accumulate in adrenal gland cells over time.
- Age and gender patterns: ACC can occur at any age but shows peaks in early childhood and again in adults (commonly in the 40s–50s). Some studies report a higher frequency of ACC in women.
Who should consider genetic testing? Patients diagnosed at a young age, those with a family history of related syndromes or multiple cancers, or those with features suggestive of an inherited condition should discuss genetic testing and counseling with their endocrinology or oncology team.
What types of medical procedures and treatments are available for adrenal gland cancer?
Treatment for adrenal gland cancer is individualized but typically centers on surgical removal (adrenalectomy). Depending on tumor type, stage, and overall health, surgery may be complemented by radiation, chemotherapy (including mitotane), targeted therapy, or hormone‑blocking medications.
Management depends on whether the tumor is localized or metastatic and whether it produces hormones. In simple terms: localized disease → surgery; unresectable or metastatic disease → systemic therapy ± radiation. Below are the main options and typical indications.
- Surgery (adrenalectomy) — the cornerstone for localized tumors:
- Laparoscopic adrenalectomy: Minimally invasive approach for smaller, noninvasive tumors. Shorter hospital stay and faster recovery.
- Open adrenalectomy: Preferred for large or invasive tumors (common for advanced adrenocortical carcinoma) to ensure complete removal and allow resection of involved tissue.
- Robotic adrenalectomy: A minimally invasive option using robotic arms for enhanced precision in select centers.
- Preoperative optimization is essential — for example, patients with pheochromocytoma (medulla tumors that make adrenaline-type hormones) require alpha‑blockade to control blood pressure before surgery.
- Radiation therapy: Used as adjuvant therapy after surgery when there’s concern about residual disease, or for symptom control for metastatic lesions. Stereotactic body radiation therapy (SBRT) can precisely target adrenal metastases in select cases.
- Chemotherapy / adrenolytic therapy: Mitotane is a drug with specific activity against adrenocortical carcinoma and is used for advanced disease or as adjuvant therapy in high‑risk cases; it requires close monitoring for side effects and blood levels. Combination chemotherapy regimens may be used for metastatic carcinoma.
- Targeted therapy and investigational treatments: Targeted drugs and clinical trials may be options for selected patients, especially when standard treatments are ineffective. Research into molecularly targeted agents for adrenal cancers is ongoing.
- Hormone‑blocking and supportive treatments: When tumors make excess hormones, medications can control symptoms (for example, antihypertensives for aldosterone excess or drugs to manage cortisol effects). Lifelong hormone replacement may be needed if both adrenal glands are removed or if adrenal insufficiency develops.
A multidisciplinary team — endocrinologist, endocrine surgeon, medical oncologist, radiation oncologist, radiologist, and specialized nursing staff — should collaborate to create the optimal plan for each patient. Discuss neoadjuvant (pre‑surgical) or adjuvant (post‑surgical) strategies with your team, and ask about clinical trials if standard options are limited.
Who is an ideal candidate for adrenal gland cancer treatment?
Ideal candidates are usually people with localized disease, good overall health to tolerate procedures, and limited or controllable spread. Final eligibility depends on tumor type, stage, and individual medical factors assessed by a multidisciplinary team.
Assessing candidacy for specific adrenal cancer treatments requires a careful review of clinical stage, tumor biology, and the patient’s medical fitness. Below is a practical checklist clinicians and patients commonly use when considering surgery or other treatments.
- Localized disease: Patients whose cancer is confined to the adrenal gland (or limited, resectable local extension) are generally the best candidates for adrenalectomy.
- Overall fitness: Good cardiac, pulmonary, and renal function improves surgical tolerance. Comorbidities should be optimized before major procedures.
- Tumor type and size: For adrenocortical carcinoma (ACC), surgery is the cornerstone—complete resection offers the best chance of cure. Large tumors may still be resectable if clear margins are achievable. Pheochromocytoma/paraganglioma require preoperative medical preparation (alpha‑blockade) because of medulla hormone effects.
- Metastatic or advanced disease: Some people with limited metastases may benefit from surgery or metastasectomy to improve symptoms or survival; others are better served with systemic therapies (chemotherapy, mitotane, targeted agents) and/or radiation.
- Response to neoadjuvant therapy: Patients whose tumors shrink with preoperative therapy may become candidates for surgery.
- Patient preferences & support: Willingness to proceed with recommended treatments, realistic expectations, and a strong support system all influence decision making.
A coordinated team—endocrinologist, endocrine surgeon, medical oncologist, radiation oncologist, anesthesiologist, and specialized nursing staff—should evaluate each case and discuss risks, benefits, and alternatives tailored to the patient’s stage and goals of care.
What is the typical recovery process after adrenal gland cancer surgery or treatment?
Recovery varies by procedure and by whether additional therapies (chemotherapy or radiation) are needed. Laparoscopic procedures usually have shorter hospital stays and faster return to normal activity; open surgery and combined treatments require longer recovery and closer hormone monitoring.
Your recovery timeline depends on the type of adrenal surgery, overall health, and whether the tumor affected hormone production. Below are typical milestones, plus practical tips for monitoring hormones and recognizing warning signs that require urgent care.
- After laparoscopic or robotic adrenalectomy:
- Hospital stay: Typically 1–3 days.
- Pain: Generally mild-to-moderate, managed with oral medications.
- Activity: Light activities within 1–2 weeks; avoid heavy lifting and strenuous exercise for 4–6 weeks.
- Return to work: Often 2–4 weeks depending on job demands.
- Full recovery: Commonly 4–6 weeks.
- After open adrenalectomy:
- Hospital stay: Often 5–7 days or longer.
- Pain: More significant initially; may require stronger analgesia before transitioning to oral meds.
- Activity: Gradual increase; avoid heavy lifting for 6–12 weeks.
- Return to work & full recovery: Often 6–12 weeks or longer based on the procedure and your body’s response.
- Hormone management and monitoring:
- If the tumor produced hormones (cortisol, aldosterone, sex steroids, or adrenaline-family hormones), your team will monitor blood tests and blood pressure closely after surgery.
- If both adrenal glands are removed or if the remaining gland is insufficient, lifelong hormone replacement (e.g., hydrocortisone, fludrocortisone) may be necessary; even after unilateral removal some patients need temporary steroid support.
- Post‑treatment surveillance: Regular follow-up visits include blood tests (hormone panels), tumor markers where applicable, and imaging scans (CT or MRI) to detect recurrence or assess treatment response.
- Emotional recovery and support: A cancer diagnosis and treatment can be stressful; consider counseling, support groups, and clear communication with your team to manage anxiety and expectations.
When to seek urgent care: Fever, uncontrolled pain, signs of infection at the incision, sudden dizziness or fainting, very low blood pressure, severe vomiting, or symptoms suggesting adrenal crisis (severe weakness, confusion, abdominal pain) require immediate medical attention.
Planning for travel (if receiving treatment abroad): Pack copies of your diagnosis, imaging, and recent blood tests; plan to stay locally for the recommended recovery period (discuss timing with your surgeon), and arrange clear follow-up plans with your home medical team before returning.
What are the potential risks and side effects associated with adrenal gland cancer treatment?
Treatments for adrenal gland cancer — including surgery, chemotherapy (such as mitotane), and radiation — carry risks ranging from surgical complications to hormonal imbalances and systemic side effects. Long-term monitoring and patient education help reduce these risks and manage side effects effectively.
Understanding likely complications and how they are prevented or treated helps you weigh risks and benefits. Below are the main categories of risks, mitigation strategies, and “red flag” signs that require urgent attention.
- Surgical risks (adrenalectomy):
- Bleeding, infection, or wound problems: Standard perioperative precautions (antibiotics, careful hemostasis) reduce risk.
- Injury to nearby organs: Rare damage to kidney, spleen, pancreas, or bowel; experienced endocrine surgeons minimize these risks.
- Blood clots (DVT/PE): Preventive measures include early mobilization and, when indicated, blood thinners.
- Hypertensive crisis (pheochromocytoma): Tumors of the adrenal medulla can release adrenaline‑type hormones during manipulation; preoperative alpha‑blockade and experienced anesthesia care are essential.
- Adrenal insufficiency: If both glands are removed or the remaining gland is suppressed, patients may need lifelong steroid replacement; teams prepare patients and teach steroid emergency protocols.
- Chemotherapy and mitotane-related effects:
- Gastrointestinal issues: Nausea, vomiting, diarrhea, and loss of appetite are common; antiemetics and supportive care help.
- Fatigue and neurologic symptoms: Dizziness, lethargy, confusion, or concentration problems can occur, particularly with mitotane.
- Liver toxicity: Mitotane and some systemic drugs require regular liver‑function monitoring.
- Bone marrow suppression and infection risk: Other chemotherapies can lower blood counts, increasing infection risk.
- Radiation therapy side effects:
- Local skin changes and fatigue: Mild-to-moderate and usually temporary.
- GI symptoms or nearby tissue effects: If the abdomen is irradiated, nausea or damage to adjacent tissues is possible; modern techniques (e.g., SBRT) aim to limit exposure.
- Long‑term and psychosocial considerations:
- Hormone imbalance and replacement: Lifelong monitoring of hormone levels and replacement therapy may be required after treatment.
- Recurrence risk: Continued surveillance with tests and imaging is important because adrenal cancer can recur.
- Mental health impact: Anxiety, depression, and fear of recurrence are common and should be addressed with counseling or support groups.
Red flags — seek immediate care: severe chest pain or shortness of breath (possible PE), very high or uncontrolled blood pressure, sudden dizziness or fainting, high fever or wound redness/drainage, severe vomiting or confusion (possible adrenal crisis). If you experience these, contact emergency services right away.
Risk mitigation tips: Ensure preoperative optimization (cardiac/pulmonary evaluation), alpha‑blockade when indicated, close monitoring of blood tests and liver function during mitotane, and clear steroid‑replacement instructions. Discuss benefits versus risks with your multidisciplinary team to make an informed choice.
How much does adrenal gland cancer treatment cost globally, and what impacts pricing?
Estimated costs for adrenal gland cancer care vary widely around the world — illustrative ranges below span roughly $10,000 to $100,000+ depending on the procedure, country, and services included. These figures are estimates; always request an itemized, up‑to‑date quote from any facility you consider.
Cost is a major factor for many patients researching adrenal cancer treatment or considering care abroad. Prices differ by country, hospital reputation, the complexity and stage of disease, and whether additional treatments (chemotherapy, radiation) or extended post‑operative care are needed. Below are illustrative ranges and the main cost drivers to discuss when comparing options.
Estimated Cost Ranges for Adrenal Gland Cancer Treatment (Surgery & Initial Care) — illustrative
| Country / RegionEstimated Range (USD)Notes | ||
| United States | $30,000 – $100,000+ | Highly variable by hospital, state, and insurance; often higher surgeon and facility fees. |
| Western Europe (e.g., Germany, UK) | $25,000 – $70,000+ | High-quality care; costs depend on public vs private pathways and self-pay pricing. |
| Turkey | $15,000 – $35,000 | Competitive pricing and international patient packages in many centers. |
| India | $10,000 – $25,000 | Often lower costs with experienced surgeons in JCI‑accredited centers; packages may include some follow-up. |
| Thailand | $12,000 – $30,000 | Strong patient services and recovery-support packages in many hospitals. |
| Mexico | $10,000 – $28,000 | Accessible option for North American patients; quality varies by center. |
Factors that influence price
- Type of procedure: Laparoscopic adrenalectomy generally costs less than open adrenalectomy due to shorter hospital stays and lower recovery needs.
- Stage and complexity: Advanced disease requiring more extensive resection (removal of surrounding tissue or organs) or multimodality treatments (chemotherapy, mitotane, radiation) raises the total cost.
- Hospital and surgeon fees: High‑volume, internationally accredited centers and very experienced surgeons often charge more but may offer better outcomes.
- Diagnostics and tests: Pre‑operative imaging (CT, MRI), hormone panels, biopsies, and repeat scans add to the total expense.
- Length of stay and follow‑up: Each extra inpatient day, postoperative medication (including hormone replacement), or separate follow‑up visit increases costs.
Practical tips when comparing costs
- Request an all‑inclusive, itemized quote that lists surgeon fees, anesthesia, hospital stay, pre/post‑op scans and tests, medications, and follow‑up care.
- Ask about accreditation (e.g., JCI), surgeon experience with adrenal tumors, complication and recurrence rates, and whether international patient coordinators provide language and logistical support.
- Factor in travel, accommodation, and a safe recovery period abroad — inexpensive surgery with inadequate follow‑up can increase overall risk and downstream costs.
These cost ranges are illustrative estimates (update and verify with facilities). For an accurate price tailored to your stage and planned treatments, request a detailed quote and discuss options with your multidisciplinary team.
Why should I consider medical tourism for adrenal gland cancer treatment?
Seeking adrenal gland cancer care abroad can provide access to specialized expertise, advanced technology, and competitively priced treatment packages in accredited centers — options that may not be available locally. With careful vetting, medical tourism can be a viable path for people who need specific treatments, shorter wait times, or cost-effective care.
For many patients, the choice to explore international treatment is not only about price but about finding the right team and facilities for their adrenal cancer. Below are common advantages, balanced with practical quality checks to reduce risk.
- Access to specialized expertise: Some centers and surgeons have high volumes of adrenal tumor cases and multidisciplinary teams experienced in adrenocortical carcinoma, pheochromocytoma, and complex adrenal surgery.
- Advanced technology and techniques: International hubs often offer robotic adrenalectomy, high-resolution imaging, and precision radiation (e.g., SBRT) that can improve surgical precision and planning.
- Potential cost advantages and bundled packages: Many accredited hospitals provide all‑inclusive packages that combine surgery, scans, medications, and some post‑op care, which can reduce overall out‑of‑pocket expense for uninsured or underinsured patients.
- Shorter wait times and coordinated care: In some systems, international patients can access consultations and scheduling faster than local public pathways, helping start time‑sensitive treatments sooner.
- Personalized support services: Many facilities offer language support, patient coordinators, and recovery packages that ease logistics for people traveling for care.
Quality assurance checklist (before you book): verify JCI or equivalent accreditation, ask for surgeon case volume and outcomes with adrenal tumors, request itemized quotes and what follow‑up is included, read patient testimonials, and confirm clear plans for post‑treatment care at home.
Medical tourism can broaden treatment options for adrenal cancer, but it requires careful planning. Discuss potential international options with your endocrine and oncology team, and ensure you have a coordinated follow‑up plan in your home country before proceeding.
Which international destinations are renowned for high-quality and affordable adrenal cancer care?
Several countries are recognized for combining internationally accredited hospitals, experienced teams, advanced technology, and competitive pricing for adrenal cancer care. These destinations often offer dedicated services for international patients, including coordinated logistics and bundled treatment packages.
When patients search for “best countries for adrenal cancer treatment” or “affordable adrenalectomy overseas,” a handful of nations commonly appear due to their balance of quality, value, and patient support. Below are typical strengths and practical expectations for each destination — remember that quality varies by hospital and surgeon, so always verify accreditation and outcomes for the specific center you are considering.
- India:
- Why: Many JCI‑accredited hospitals with endocrine and oncology centers of excellence and experienced surgeons managing adrenal tumors and adrenocortical carcinoma (ACC).
- What to expect: Competitive pricing, comprehensive international patient services, English‑speaking staff, and bundled packages that may include surgery, scans, and some follow‑up.
- Turkey:
- Why: Rapidly growing medical tourism sector with modern facilities and many internationally accredited hospitals experienced in complex abdominal and endocrine surgery.
- What to expect: State‑of‑the‑art surgical suites, experienced surgeons, and coordinated care packages for international patients.
- Thailand:
- Why: Strong reputation for patient experience, JCI‑accredited hospitals, and a service‑oriented approach to international care.
- What to expect: High level of patient hospitality, comprehensive recovery support, and modern diagnostic and surgical technology.
- Mexico:
- Why: Convenient option for many North American patients with growing centers of excellence and surgeons trained in U.S. systems.
- What to expect: Shorter travel time for U.S. and Canadian patients, bilingual staff in many centers, and competitive pricing — verify center accreditation and surgeon experience.
- South Korea:
- Why: Noted for advanced medical technology, research, and strong outcomes in complex surgeries and oncology care.
- What to expect: Very high technical standards and innovation; costs can be higher than other medical tourism destinations but still competitive compared with Western prices.
How to vet a center: Verify JCI or equivalent accreditation, ask about surgeon volumes and specific experience with adrenal tumors and ACC, request complication and recurrence statistics if available, check patient testimonials, and confirm what is included in any package (scans, tests, follow‑up).
What should I expect when traveling for adrenal cancer treatment abroad, and how can I ensure safety and quality?
Traveling for adrenal cancer care requires planning both medical and logistical details — from sharing diagnostic scans and tests to arranging visas and a recovery plan. To protect your safety, choose accredited hospitals, verify surgeon credentials, request itemized treatment quotes, and confirm post‑treatment follow‑up with your home team.
A successful international treatment journey hinges on careful preparation and clear communication. Below is a practical checklist of what to expect, how long to plan to stay, and steps to verify quality before you travel.
Before you travel (checklist)
- Collect and share medical records: Send recent imaging (CT/MRI scans), blood and hormone test results, pathology reports, and letters from your local doctors to the international center for a pre‑travel assessment.
- Request an itemized treatment plan and quote: Ensure the quote lists surgeon and hospital fees, anesthesia, scans/tests, medications (including mitotane if indicated), length of stay, and follow‑up care so you can compare offers accurately.
- Verify credentials and quality: Confirm JCI or equivalent accreditation, ask about surgeon volume with adrenal tumors and adrenocortical carcinoma, and request complication/recurrence data where available.
- Plan recovery time: Discuss with the surgical team how long you should stay locally after the procedure (typical guidance: laparoscopic 7–14 days; open surgery often several weeks — follow your surgeon’s advice).
- Arrange logistics: Confirm visa requirements, accommodation, airport transfers, language support, and whether the facility provides an international patient coordinator.
What to expect on arrival and during treatment
- Local medical evaluation: Expect repeat physical exams and possibly repeat scans or hormone panels to confirm the diagnosis and staging before proceeding.
- Coordinated care pathway: Your international team should provide a clear timeline for preoperative tests, surgery (if indicated), post‑op care, and discharge planning.
- Recovery and monitoring: Hospitals typically monitor blood pressure, hormone levels (cortisol, aldosterone, etc.), and wound healing; ensure you understand signs that need urgent attention.
- Post‑treatment documentation: Request copies of operative notes, pathology, medication instructions (including steroid replacement plans if applicable), and a follow‑up schedule to share with your home team.
How to ensure safety and quality — practical steps
- Check accreditation and outcomes: Look for JCI or equivalent accreditation and ask specifically about surgeon experience with adrenal tumors and adrenocortical carcinoma.
- Verify facilitator credentials: If using a medical tourism facilitator, confirm their reputation, ask for references, and ensure they provide transparent information about hospitals and clinicians.
- Communication plan: Confirm language support and a dedicated point of contact at the hospital; ensure your home doctor is looped into post‑op care.
- Legal and insurance considerations: Understand the destination country’s medical liability environment and whether travel or medical evacuation insurance is recommended.
Preparing questions for the surgical team — Ask about expected hospital stay, surgeon volume with adrenal procedures, expected scans/tests during your stay, how hormone replacement will be handled, and the plan if complications arise.
Careful planning and clear communication between you, your international team, and your home providers can make medical travel for adrenal cancer a safe and effective option. Always follow your surgeon’s recommendations about local recovery time before flying home, and keep all diagnostic scans and test results with you when traveling.
Take the Next Step with DGS Healthcare
Ready to explore adrenal cancer treatment options abroad? Compare accredited clinics, review surgeon experience with adrenal tumors, and receive a tailored, itemized quote to help you make an informed decision.
When you request a quote you’ll be asked to share basic medical details (diagnosis, recent scans/tests) so hospitals can provide accurate estimates; DGS Healthcare can also help verify accreditation and clinician credentials.
