Brachytherapy – Internal Radiation Therapy
Brachytherapy is a highly targeted internal radiation therapy where small radioactive sources are placed directly inside or next to the tumor. By delivering a focused dose of radiation to cancer cells while limiting exposure to nearby healthy tissue, brachytherapy offers an effective, often less invasive option for select cancers — commonly prostate (LDR seed implants), cervical (HDR afterloading), and some breast cancers.
Brachytherapy: Pinpointing Cancer with Internal Radiation Therapy
A cancer diagnosis brings many decisions. One option your oncology team may discuss is brachytherapy — also called internal radiation therapy — which places radioactive sources inside the body near the tumor so the highest radiation dose hits the cancer directly. This “inside body” approach can reduce collateral radiation to surrounding organs compared with external beam radiation therapy.
Brachytherapy is a type of radiation treatment that can be delivered in different ways (see types of brachytherapy later). For example, low-dose-rate (LDR) prostate treatment uses permanently implanted seeds that emit radiation over months, while high-dose-rate (HDR) treatments use temporary sources placed through applicators for minutes at a time. The choice depends on the tumor location, size, stage, and overall health.
If you’re researching “what is internal radiation,” “benefits of brachytherapy,” or “brachytherapy recovery,” a good next step is to talk with your radiation oncology team about whether this targeted therapy fits your diagnosis and goals. Reputable guidelines (for example, professional societies like ASTRO or national cancer networks) can provide evidence-based recommendations to discuss with your care team.
What symptoms might indicate a need for Brachytherapy?
Symptoms that could lead to a discussion about brachytherapy are those caused by the cancer itself (for example, urinary changes with prostate cancer or abnormal vaginal bleeding with cervical cancer). Remember: brachytherapy is a treatment for an established cancer diagnosis, not a diagnostic test.
Because brachytherapy treats localized tumors, the signs that bring someone to a doctor are the typical symptoms of the underlying cancer. Below are common cancers treated with brachytherapy and the symptoms that commonly prompt evaluation. If you notice any of these, see a healthcare professional for screening and diagnosis — the pathway is usually screening → diagnostic tests (imaging/biopsy) → multidisciplinary treatment planning.
- Prostate Cancer: Symptoms may include frequent or difficult urination, weak stream, blood in urine or semen, and erectile difficulties. Early prostate tumors are often found with screening (PSA, digital rectal exam) rather than symptoms; brachytherapy (LDR seeds or HDR) is an option for many localized cases.
- Cervical Cancer: Look for abnormal vaginal bleeding (between periods, after sex, or after menopause), unusual discharge, pelvic pain, or pain during intercourse. Persistent abnormal bleeding should prompt evaluation — most cervical cancers are linked to HPV infection, so screening with Pap tests and HPV testing is key.
- Breast Cancer: A new lump, changes in breast shape or skin, nipple inversion or unusual discharge are common reasons for imaging and biopsy. For select early breast tumors, partial-breast brachytherapy may be an option.
- Skin (Non-melanoma) Cancer: New or changing skin lesions, sores that don’t heal, or suspicious moles — some superficial skin tumors can be treated with local brachytherapy approaches.
- Head and Neck Cancers: Persistent sore throat, difficulty swallowing, voice changes, or a neck lump warrant evaluation; brachytherapy can be used for certain localized lesions.
If you notice concerning signs, contact your doctor. After diagnostic confirmation (imaging and biopsy), a multidisciplinary team — including radiation oncologists and medical physicists — will determine whether internal radiation therapy like brachytherapy suits your tumor’s size, location, and stage.
What causes the cancers commonly treated by Brachytherapy?
Causes vary by cancer type but generally include genetic mutations, lifestyle factors (like smoking or alcohol), infections (notably HPV for cervical cancer), hormones, and environmental exposures. Understanding risk factors helps with prevention and early detection.
Cancer development is complex and multifactorial. Below are commonly recognized risk factors for cancers often treated with internal radiation therapy. Where relevant, screening and preventive measures can reduce risk or enable earlier detection.
- Prostate Cancer: Risk rises with age (most cases after 50), family history, and certain ethnic backgrounds (higher incidence in African American men). Lifestyle factors such as obesity and diet are associated but are not direct causes. Regular screening discussion is recommended for men at risk.
- Cervical Cancer: Persistent infection with high-risk human papillomavirus (HPV) is the main cause; HPV vaccination and routine Pap/HPV screening are effective prevention strategies. Smoking and immune suppression increase risk.
- Breast Cancer: Factors include age, genetic mutations (BRCA1/BRCA2), reproductive history, certain hormone exposures, alcohol use, and obesity. Genetics raises risk substantially in a minority of patients.
- Skin Cancer: UV radiation exposure from the sun or tanning beds is the primary cause; fair skin and immunosuppression increase vulnerability.
While some risk factors can’t be changed (age, genetics), many can be reduced through vaccination, avoiding tobacco, limiting alcohol, maintaining healthy weight, and following screening recommendations. For specific prevention and screening guidance, consult your primary care provider or oncology team and refer to national cancer guidelines.
What are the different types of Brachytherapy?
Brachytherapy is classified by dose rate (High-Dose Rate – HDR, Low-Dose Rate – LDR) and by whether the radioactive source is temporary or permanent. HDR gives short, intense doses; LDR uses continuously emitting seeds over weeks or months.
Different types of brachytherapy are chosen based on tumor location, size, and treatment goals. Below are the main approaches and what patients can typically expect.
- High-Dose Rate (HDR) Brachytherapy:
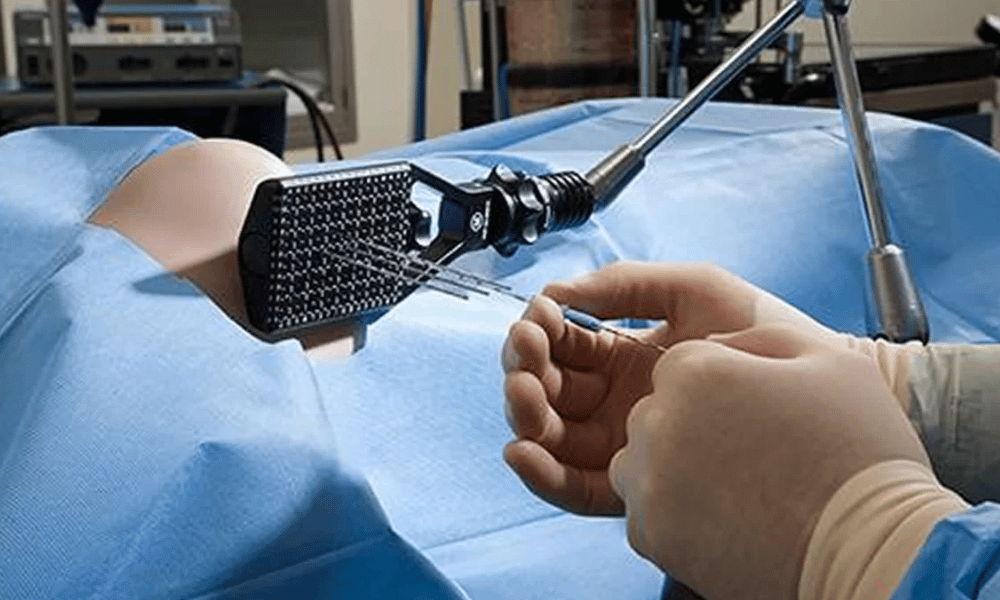
- How it works: A strong radioactive source (commonly Ir-192) is temporarily driven into place through thin catheters or an applicator. The source dwells for minutes at planned positions to deliver the prescribed dose.
- Treatment schedule: Multiple short sessions are typical — for example, several fractions given over a few days or weeks, often outpatient.
- Advantages: Precise dose radiation, flexible dosing, and no residual radioactivity in the body between treatments. HDR is commonly used for cervical, breast, prostate, lung, and esophageal tumors.
- Keywords/search terms: “HDR”, “minutes”, “temporary internal radiation.”
- Low-Dose Rate (LDR) Brachytherapy:
- How it works: Tiny radioactive seeds (e.g., I-125, Pd-103) are permanently implanted into or near the tumor and emit radiation continuously over weeks to months as their activity decays.
- Treatment schedule: Usually a single implant procedure — common for certain prostate cancers.
- Advantages: One-time procedure, continuous dose to the tumor, and minimal visits afterward; may require brief precautions about close contact with pregnant women or young children until activity decays.
- Keywords/search terms: “LDR”, “seeds”, “permanent seed implant”, “weeks”, “months”.
- Pulsed-Dose Rate (PDR) Brachytherapy:
- How it works: Uses a remote afterloading machine to deliver radiation in frequent short pulses, combining some biological advantages of LDR with the control of HDR.
- Treatment schedule: Often delivered over one to two days in a hospital setting, depending on the plan.
Which type is best depends on tumor stage, location, patient anatomy, and goals. A multidisciplinary team evaluates dose, rate, applicator placement, and expected side effects to choose HDR, LDR, or PDR. For many patients, brachytherapy can be combined with external beam radiation when a higher total dose or broader coverage is needed.
Who is a good candidate for Brachytherapy?
A good candidate for brachytherapy usually has a well-defined, localized tumor that can be reached safely with applicators or implants. Eligibility depends on cancer type, tumor size and location, stage, and the patient’s overall health and preferences.
Decisions about internal radiation therapy are made by a multidisciplinary team — typically including a radiation oncologist, medical oncologist, surgeon, and medical physicist — who review imaging, pathology, and your general health. Key factors the team considers include:
- Cancer type and stage: Brachytherapy is most useful for localized solid tumors — commonly early-stage prostate, cervical, and certain breast cancers — and in some head & neck, skin, and gynecologic cases.
- Tumor size and accessibility: The tumor must be accessible for precise placement of radioactive sources or applicators; very large or diffuse tumors are less suitable.
- Anatomy and nearby organs: The position of critical structures (bladder, rectum, nerves) affects safety and planning; applicator placement must avoid undue risk.
- Prior treatments: Brachytherapy can be a primary treatment, a boost after external beam radiation, or an option for recurrence in selected cases.
- Overall health and anesthesia risk: Patients should be fit for the procedure; some forms (HDR or PDR) may require brief hospital stays or anesthesia.
- Patient preference: After discussing risks, benefits, and alternatives (including external beam radiation, surgery, or combined approaches), the patient’s informed choice is central.
Common patient questions include “is brachytherapy right for me?” and “who qualifies for internal radiation?” For example, many men with early-stage, low- to intermediate-risk prostate cancer are good candidates for LDR seed implants, while women with locally advanced cervical cancer often receive HDR brachytherapy as part of definitive treatment.
What is the recovery like after Brachytherapy?
Recovery varies by type and site: HDR patients often return to normal activity quickly between short sessions, while LDR implant patients recover from a surgical implant and may have a slightly longer initial healing period.
Overall, recovery after brachytherapy is typically less extensive than major surgery, but timelines differ by approach and treated body area. Typical expectations:
- HDR (temporary sources): Immediate post-procedure symptoms often include mild pain at the site and fatigue. Sessions are short (minutes per dwell), often outpatient, and there’s no ongoing radioactivity in your body. Most people resume normal activities within days to a few weeks after the final session.
- LDR (permanent seeds/implants): Because seeds are implanted surgically, expect localized soreness, swelling, or bruising after the procedure, and brief activity restrictions (a few days to a week). The seeds emit radiation over weeks to months as their activity declines; short, temporary precautions about close contact with pregnant women or very young children may be advised.
Practical tips: pack comfortable clothing, arrange a ride home for the day of the procedure, and confirm with your team how long you may need to stay in hospital or abroad for follow-up. Always ask your provider for a personalized recovery timeline and restrictions.
What are the potential risks and side effects of Brachytherapy?
Although brachytherapy is highly targeted, it can cause side effects — most are localized to the treated area and are manageable. Typical issues include irritation, swelling, fatigue, and organ-specific effects such as urinary or bowel changes after prostate treatment.
All radiation treatments carry risks. Because brachytherapy places the radioactive source near the tumor, it often reduces collateral radiation to the rest of the body, but side effects vary by site and by whether the approach is HDR, LDR, or PDR. Below is a practical “what to expect” breakdown and guidance on managing common effects.
- Common, short-term effects (across sites):
- Fatigue: Frequently reported but usually mild and temporary; rest and gradual activity increase help recovery.
- Local pain or discomfort: At the implant or applicator site; typically controlled with simple analgesics.
- Swelling or bruising: More common after LDR implants; usually resolves over days to weeks.
- Infection: Rare but possible at insertion sites — contact your care team for increasing pain, fever, or drainage.
- Site-specific effects and practical management:
- Prostate brachytherapy: Urinary symptoms (frequency, urgency, burning, weak stream) and bowel changes (rectal irritation, urgency) are common early on. Erectile dysfunction can occur months to years later in some patients. Management includes medications, pelvic floor exercises, and specialist follow-up.
- Cervical brachytherapy: Vaginal irritation, dryness, or narrowing, plus urinary or bowel irritation and fatigue — vaginal dilator therapy and pelvic rehabilitation may be recommended long term.
- Breast brachytherapy: Local soreness, swelling, skin changes (redness, induration), and occasional cosmetic changes; wound care and topical treatments help symptoms.
Long-term effects are less common but can occur (for example, some patients experience persistent urinary or sexual function changes after prostate brachytherapy). Ask your team for expected rates of long-term effects for your specific tumor type — many centers can provide outcome statistics. Typical recovery and resolution timelines range from weeks to months, depending on the effect and treatment type.
Red flags — contact your care team or seek urgent care if you experience high fever, uncontrolled bleeding, severe pain not relieved by medications, or signs of infection at an implant site. Your oncology team will also give tailored advice about any temporary precautions (for example, limited close contact with pregnant women or young children for a short period after certain LDR implants).
How much does Brachytherapy cost globally?
The cost of brachytherapy varies widely worldwide — from tens of thousands of dollars in high-cost health systems to a fraction of that price in popular medical tourism destinations like India, Mexico, and Turkey. Differences reflect healthcare systems, technology, staffing, and what’s included in the quoted package.
Cost is an important factor when comparing treatment options. Prices depend on the type of brachytherapy (HDR vs. LDR), tumor complexity, number of sessions, inpatient stay requirements, and the clinic’s reputation. The table below gives approximate ranges; these are estimates and should be confirmed with specific hospitals or international patient departments (ranges as of 2024).
| CountryEstimated Brachytherapy Cost (USD)Notes on Cost Factors | ||
| United States | $30,000 – $80,000+ | Higher unit costs, advanced tech, and often bundled services vary by insurance coverage and facility. |
| United Kingdom | $20,000 – $50,000 | Public systems may cover residents; private international patients pay market rates. |
| Germany | $25,000 – $60,000 | High-quality care and advanced centers; costs reflect facility and staffing levels. |
| India | $5,000 – $15,000 | Lower labor and operational costs; many JCI-accredited centers and competitive packages. |
| Mexico | $7,000 – $20,000 | Close to North America; many clinics offer travel packages and bilingual staff. |
| Turkey | $8,000 – $22,000 | Modern facilities and experienced specialists, often competitively priced for international patients. |
| South Korea | $15,000 – $40,000 | High-tech centers and strong research programs; pricing reflects advanced infrastructure. |
Note: Estimates may exclude travel, accommodation, translator services, and extended post-procedure care unless explicitly included. Always request an itemized quote that covers pre-op testing, the procedure, hospital stay (if any), implants or sources, and follow-up.
When comparing options, ask these questions: Does the quote include anesthesia and operating room fees? How many HDR sessions or LDR implants are included? Who is on the treating team and what are their outcome statistics? What follow-up care is provided, and how long might you need to stay in the hospital or country for initial checks? These details affect total cost and your recovery timeline.
Why consider Brachytherapy abroad for treatment?
Patients often consider treatment abroad to reduce costs, access specialized teams and technology, shorten waiting times, or take advantage of integrated treatment packages that simplify logistics.
Medical tourism can deliver significant savings for brachytherapy while providing high standards of care in many accredited international centers. Balance financial benefits against travel, communication, and post-treatment follow-up needs; verify hospital accreditation (e.g., JCI), physician credentials, and transparent pricing before deciding.
What should I expect when traveling abroad for Brachytherapy?
When you travel abroad for brachytherapy, anticipate coordinated planning of medical records, travel logistics, and short-term accommodation. On arrival you’ll have in-person consultations, undergo the procedure, and receive post-treatment instructions — often with support from an international patient coordinator or medical tourism facilitator.
Medical travel for cancer treatment can be manageable with good preparation. Below is a practical timeline and checklist so you know what to expect from initial contact through follow-up.
- Pre-trip: initial consultation & planning
- Remote evaluation: Send your scans, pathology reports, and prior treatment notes so the treating team can review and recommend HDR, LDR, or PDR options and an estimated plan.
- Logistics: Coordinate visas, flights, accommodation, and local transfers. Confirm whether the quote includes hospital room, implants or seeds, anesthesia, and follow-up visits.
- Insurance & costs: Check medical travel insurance and get an itemized cost breakdown (procedure, team fees, imaging, hospital stay).
- Arrival & pre-treatment
- On-site consultations: You’ll meet the multidisciplinary team (radiation oncologist, medical physicist, surgeon) who confirm the plan, applicator or implant approach, and expected stay.
- Pre-op testing: Expect blood tests, imaging, and anesthetic assessment; the team will explain any temporary restrictions (e.g., fasting, medications).
- The procedure
- What happens: HDR sessions use an applicator and short source dwell times (minutes); LDR involves implantation of seeds in a single procedure. Depending on the approach, you may need only outpatient visits or a brief hospital stay.
- Hospital stay & room: HDR is often outpatient or short stay; LDR may require overnight observation. Confirm room arrangements and recovery support with the clinic.
- Post-treatment & departure
- Recovery instructions: The team will give written guidance on wound care, activity restrictions, and symptom management; keep emergency contact details.
- Follow-up: Discuss how long you must remain in-country for initial follow-up and whether future checks will be remote or coordinated with your local doctors.
- Return home: Bring all documentation, imaging, and a clear plan for ongoing care with your home oncology team.
Practical tips: pack medical records and a list of medications, arrange a responsible person to travel with you if possible, check visa and vaccination requirements, and buy travel medical insurance that covers complications. Confirm language support or translator availability so you can communicate clearly with the treatment team.
How can I ensure safety and quality for Brachytherapy abroad?
Choose internationally accredited hospitals (for example, JCI), verify the treating team’s credentials, demand transparent pricing, read independent patient reviews, and confirm post-treatment follow-up arrangements to protect your safety and outcomes.
Steps to reduce risk include:
- Check accreditation and outcomes: Look for JCI or similar accreditation and ask the hospital for aggregated outcome data for the specific brachytherapy procedure.
- Verify the team: Confirm the radiation oncologist, medical physicist, and operating team credentials and experience with the specific applicator or implant technique.
- Demand transparent quotes: Ensure the price includes the implants or seeds, operating room, imaging, hospital room, and follow-up; ask who covers complications or re-admissions.
- Use reputable facilitators carefully: If using a medical tourism agency, verify their vetting process and prefer clinics with verifiable accreditation and independent reviews.
- Plan follow-up with your home team: Ensure your local doctor will coordinate remote follow-up and that you understand who manages late effects or complications.
Following these steps helps ensure a safer, more predictable experience when seeking brachytherapy abroad. If in doubt, obtain a second opinion from a trusted local specialist before traveling.
Are there patient success stories for Brachytherapy from abroad?
Yes — many patients report positive experiences and good clinical outcomes after traveling for brachytherapy. Testimonials commonly highlight effective tumor control, shorter wait times, cost savings, and supportive care from international teams.
While individual stories are encouraging, remember they are anecdotal and outcomes vary by diagnosis, tumor stage, and the treating team’s expertise. Ask clinics for aggregated outcome data and published results when evaluating international centers. Below are common themes seen in patient-reported experiences.
- Cost-savings enabling treatment: Many patients describe accessing high-quality brachytherapy abroad (including implants or seeds) at a lower overall cost, which made timely treatment possible.
- Faster access to care: For patients facing long domestic wait times, traveling for treatment often meant quicker initiation of therapy, which can be important for tumor control.
- Experienced teams and technology: Patients frequently cite confidence in multidisciplinary teams (radiation oncologists, medical physicists, surgeons) and modern equipment as reasons for good outcomes.
- Compassionate care and coordination: Positive reports often note helpful international patient coordinators, translators, and clear follow-up plans that eased the journey.
- Clinical outcomes: Some patients achieve durable tumor control or remission after brachytherapy abroad, especially for well-selected localized tumors like prostate, cervical, or select breast cancers — but results depend on many factors and are not guaranteed.
How to evaluate testimonials: request anonymized outcome statistics, verify physician credentials, confirm facility accreditation (e.g., JCI), and ask how the international team coordinates follow-up with your local oncologist. These steps help turn encouraging stories into verified evidence you can trust when choosing a treatment team.
Take the Next Step with DGS Healthcare
Ready to explore brachytherapy treatment options abroad? Compare accredited clinics and international hospital teams, review cost estimates, and get a free, personalized quote to help plan your medical travel.
DGS Healthcare collects only the information needed to provide quotes and connects you with vetted providers. For detailed questions, request clinic outcome data and follow-up arrangements before booking.
