Brain Cancer Treatment
Brain cancer treatment involves various approaches like surgery, radiation, and chemotherapy, often performed abroad for cost savings or access to specialized care, offering hope and advanced therapies for patients globally.
Navigating Brain Cancer: Advanced Treatments & Global Care Options
A diagnosis of brain cancer is life-changing and raises many urgent questions about prognosis and next steps. Brain cancer — also called a brain tumor — is an abnormal growth of cells in the brain: some are benign, many are malignant, and outcomes vary widely depending on the tumor type and grade. While each person’s situation is unique, advances in surgery, radiation, and targeted therapies have improved survival and quality of life for many people.
Many patients explore options beyond their home country to access specialized expertise or lower-cost care. Medical tourism for brain cancers can provide access to technologies or specialists not locally available, sometimes at lower cost, but it also requires careful planning. This guide explains common symptoms and diagnosis steps, treatment options (surgery, radiation, chemotherapy, targeted and immune therapies), recovery and risks, and practical tips for seeking treatment abroad.
If you are preparing for an international consultation, bring copies of your key medical records — MRI scans, pathology reports, a current medication list, and your treating physician’s notes — so specialists can review your case and recommend appropriate treatment pathways. Continue reading to learn what to expect and how to evaluate options for you or a loved one.
What are the Symptoms of Brain Cancer?
Symptoms of brain cancer vary depending on the tumor’s size, location, and growth; common complaints include persistent headaches, new-onset seizures, vision changes, and shifts in personality or coordination.
Early recognition of symptoms can speed diagnosis, but many signs are non-specific and overlap with other conditions. Symptoms typically result from increased intracranial pressure or from a tumor affecting a particular brain region or nerve pathway. Below are common symptoms and why they happen.
- Persistent Headaches: Often different from usual headaches — worse in the morning or progressively increasing, sometimes with nausea or vomiting due to raised pressure.
- Seizures: New-onset seizures are a common presenting symptom in adults and can range from generalized convulsions to brief focal twitches or sensory changes.
- Vision Problems: Blurred or double vision, loss of peripheral vision, or visual field cuts — often seen when tumors press on visual pathways.
- Numbness or Weakness: Weakness or sensory loss on one side of the body, balance difficulties, or coordination problems when motor or sensory areas are involved.
- Speech Difficulties: Slurred speech, trouble finding words (aphasia), or changes in language function when the dominant hemisphere is affected.
- Personality or Behavioral Changes: Frontal-lobe tumors commonly cause mood swings, poor judgment, memory problems, or changes in social behavior.
- Nausea and Vomiting: Especially when persistent without another clear cause — can reflect increased intracranial pressure or changes in cerebrospinal fluid dynamics.
- Hearing Problems: Tinnitus or hearing loss may occur with tumors near the temporal lobe or auditory nerve.
When to see a doctor: seek urgent evaluation if you develop sudden severe headaches, new seizures, rapid vision loss, sudden weakness, or any rapidly worsening neurological sign. For routine neurology visits, bring a timeline of symptom onset, copies of recent MRI scans, pathology reports (if available), a current medication list, and notes from your primary physician to help with diagnosis and management.
What Causes Brain Cancer and What are the Risk Factors?
The exact causes of most primary brain tumors are not known. Identified risk factors include certain inherited genetic syndromes, prior high-dose radiation to the head, and conditions that weaken the immune system, while many cases occur without any clear external trigger.
People often ask, “what causes brain cancer?” For primary brain tumors (those that start in the brain), researchers believe that DNA mutations in brain cells — often glial or other supporting cells of the nervous system — drive abnormal growth. Unlike some cancers, lifestyle factors such as diet or smoking have not been consistently linked to most primary brain tumors. It’s also important to distinguish primary brain tumors from metastatic tumors that spread to the brain from cancer elsewhere in the body.
Known risk factors and considerations include:
- Age and Type: Risk for many types of brain tumors increases with age, though some tumor types (for example certain embryonal tumors) are more common in children.
- High-dose Radiation Exposure: Prior therapeutic radiation to the head (for example decades earlier) is associated with an increased risk of later brain tumors; the association is strongest with high-dose exposures.
- Inherited Genetic Syndromes: A minority of tumors are linked to inherited conditions such as Neurofibromatosis Types 1 and 2, Li-Fraumeni syndrome, Von Hippel-Lindau disease, and Tuberous Sclerosis.
- Weakened Immune System: Immunocompromised individuals (for example people with HIV/AIDS or organ transplant recipients) have higher risk for certain brain lymphomas.
- Family History: Although most cases are sporadic, a family history of brain tumors may modestly increase risk and is a reason to discuss genetic counseling.
Some commonly asked concerns — such as whether stress or routine cell phone use cause brain tumors — are not supported by strong, consistent scientific evidence. Research continues into how blood supply, cerebrospinal fluid dynamics, and cellular factors influence tumor growth. If you have a personal or family history of cancer, consider speaking with a genetic counselor to review your risk and whether testing is appropriate.
What Types of Brain Cancer Treatments Are Available?
Brain cancer treatment options are broad — from surgery and radiation therapy to chemotherapy, targeted drugs, immunotherapy, and tumor treating fields (TTFields). Most plans use a combination tailored to the tumor type, grade, and the patient’s overall health.
Choosing the right treatment depends on the tumor’s type (for example gliomas, meningiomas, or metastatic lesions), its grade, size, location, and the patient’s goals. Below are common modalities, with a brief note on when each is used and how they may be combined as multimodal therapy.
- Surgery (Craniotomy): Often the first option when the tumor is accessible. Surgery aims to remove as much tumor as safely possible, relieve pressure, and provide tissue for diagnosis (histology and molecular testing). Extent of resection can affect prognosis and subsequent treatment choices.
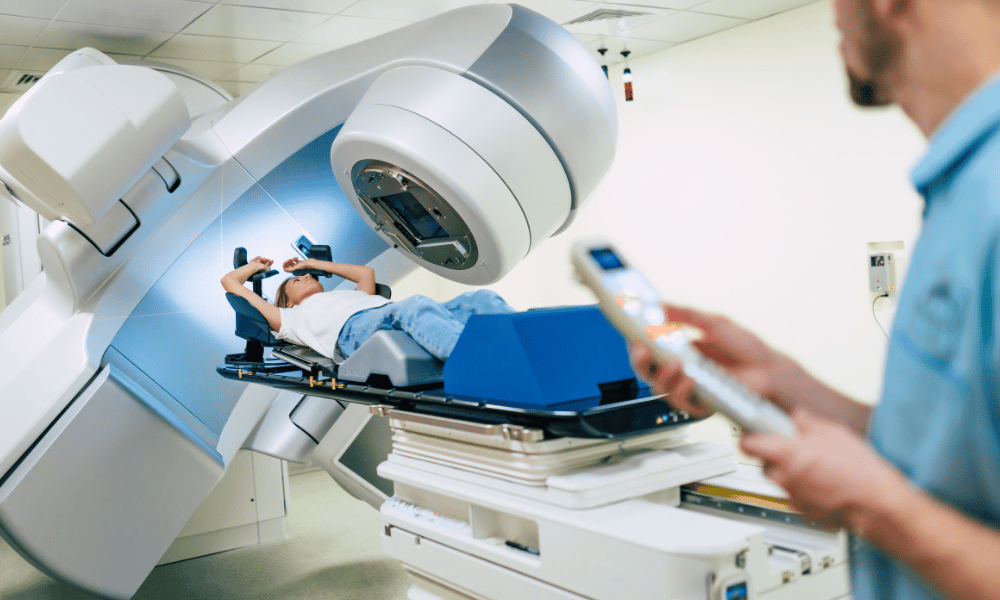
- Radiation Therapy: Uses high-energy beams to kill or control tumor cells. Options include conventional external beam radiation, stereotactic radiosurgery (Gamma Knife or LINAC-based), and proton therapy for select cases where sparing normal tissue is critical.
- Chemotherapy: Systemic drugs such as temozolomide (commonly used for glioblastoma) may be given orally or intravenously. Chemotherapy is often used alongside radiation or as maintenance therapy depending on tumor type and molecular markers.
- Targeted Drug Therapy: Targets specific molecular abnormalities in cancer cells (for example drugs that act on mutated pathways seen in some gliomas). Targeted therapy can limit damage to healthy cells compared with traditional chemotherapy.
- Immunotherapy: Treatments that harness the immune system (such as checkpoint inhibitors or vaccine approaches) are an active area of research and are approved for certain tumor types or in clinical trials.
- Tumor Treating Fields (TTFields): A non-invasive modality that uses alternating electrical fields to disrupt cancer cell division; approved for select high-grade gliomas in combination with chemotherapy.
- Rehabilitation and Supportive Care: After primary treatment, rehabilitation (physical, occupational, speech therapy) and supportive care (pain control, steroid management for edema, seizure control) are essential to restore function and quality of life.
Multimodal treatment — combining surgery, radiation, and systemic therapy — is common, especially for aggressive tumors like glioblastoma. Treatment plans increasingly rely on molecular testing of tumor cells (for example IDH mutation status in gliomas) to personalize therapy and improve outcomes. If surgery is not feasible because of tumor location, stereotactic radiosurgery or systemic options may be prioritized; discuss tumor-specific treatment options and goals with your multidisciplinary team.
Who is Eligible for Brain Cancer Treatment? (Eligibility Criteria)
Eligibility for brain cancer treatment depends on tumor characteristics (type, size, location, grade), the patient’s overall health and neurological function, age, prior treatments, and the individual’s goals for care.
Deciding who can undergo a particular therapy—such as tumor surgery, radiation, or chemotherapy—is made by a multidisciplinary team (neurosurgeon, neuro-oncologist, radiation oncologist, and neurologist). Key factors that guide eligibility include the following:
- Tumor characteristics:
- Type and grade: Different types (e.g., glioma, meningioma, metastatic lesions) and grades respond differently to treatments; high-grade tumors usually require more aggressive, combination therapy.
- Location: Tumors in accessible parts of the brain are more amenable to surgery; lesions near critical nerve centers may favor non-surgical approaches like stereotactic radiosurgery.
- Size: Larger tumors or those causing mass effect may require staged or combined treatments (debulking surgery plus radiation).
- Patient’s overall health and performance status: Clinicians commonly use ECOG or Karnofsky scores to estimate whether a person can tolerate surgery, radiation, or systemic therapy (for example, ECOG 0–2 or higher Karnofsky scores often indicate better tolerance for standard treatments).
- Age: Age alone is not an absolute barrier, but older people may have more comorbidities that influence the choice and intensity of therapy.
- Neurological function: The extent of existing deficits (speech, motor, cognitive) helps determine whether surgery or less invasive options are advisable.
- Previous treatments and tumor recurrence: A recurrent tumor’s prior treatments (surgery, radiation, chemo) narrow future options and influence eligibility for re-treatment or clinical trials.
- Patient goals and preferences: Treatment should align with the person’s priorities—curative intent, life-extension, symptom control, or quality of life—so shared decision-making is essential.
A typical decision flow is: confirm diagnosis with imaging and pathology → multidisciplinary tumor board review → assess surgical feasibility → recommend adjuvant radiation or systemic therapy as indicated. If aggressive treatment is unlikely to improve outcomes or would significantly reduce quality of life, palliative care focusing on symptom management and support may be recommended.
If you or a family member has a personal or family history of brain tumors, ask about genetic counseling and testing. Seeking a second opinion—especially for complex or high-grade tumors—is common and advisable. Bring your MRI scans, pathology reports, and a list of current medications to consultations to help teams determine the best personalized treatment plan.
What is the Recovery Time and What Can I Expect After Brain Cancer Treatment?
“Brain tumor surgery recovery time” varies from weeks to months and often requires rehabilitation to address neurological deficits; “life after brain cancer treatment” centers on recovery, ongoing monitoring, and support for the whole person.
Recovery timelines depend on the treatment type, tumor location and size, and the patient’s baseline health. Some people recover quickly from minimally invasive procedures, while others need months of rehabilitation after major surgery, radiation, or combination therapy. Below is a practical overview of what to expect and tips to support recovery and follow-up care.
- Post-surgery recovery:
- Immediate (hospital stay): Most patients stay from a few days up to a week depending on the procedure and complications. Expect swelling, headaches, fatigue, and short-term cognitive changes; steroids and pain control are commonly used.
- Short-term (first weeks at home): Rest is critical. Gradually increase activity as advised. Common symptoms include headaches, nausea, mood swings, and sleep disturbances. Seizure precautions may apply if seizures were a presenting symptom.
- Long-term (months): Full functional recovery can take several months. Rehabilitation — physical therapy for strength and balance, occupational therapy for daily tasks, and speech therapy for communication issues — often speeds recovery and improves independence.
- Recovery after radiation and chemotherapy: These therapies can cause cumulative fatigue, nausea, hair loss, and cognitive effects (“brain fog”) that may persist for weeks to months after treatment ends. Blood counts should be monitored as chemotherapy can reduce white cells, red cells, and platelets.
- Emotional and psychological impact: Anxiety, depression, and adjustment difficulties are common. Counseling, cognitive rehabilitation, and support groups can help patients and families cope and improve quality of life.
- Follow-up care and monitoring: Regular MRI scans and clinical evaluations are essential to detect recurrence early and to manage late effects (hormonal problems, hearing loss, cognitive changes). Your team will schedule a follow-up plan tailored to your tumor type and treatments received.
Practical checklist for patients and caregivers: keep a list of current medications; bring copies of operative and pathology reports to follow-up visits; arrange a contact list of treating clinicians; prepare mobility aids if needed; and plan for gradual return to travel only after medical clearance (important when treatment was received abroad — coordinate continuity of care with your local team).
Many people regain meaningful function and quality of life, though some may have permanent deficits depending on tumor location and treatment intensity. A coordinated rehabilitation and support plan, along with close follow-up, improves recovery and survivorship outcomes.
What are the Risks and Side Effects of Brain Cancer Treatment?
Risks of brain surgery include infection, bleeding, and neurological deficits. Side effects of radiation and chemotherapy can include fatigue, hair loss, nausea, lowered blood counts, and potential long-term cognitive changes.
All treatments carry risks because the brain controls essential functions. Understanding likely complications and steps to manage them helps you make informed decisions with your care team. Below is a practical breakdown of common risks and helpful measures to reduce their impact.
- Risks of Brain Surgery:
- Infection: Can occur at the incision site or intracranially. Preventive antibiotics and sterile technique reduce risk; report fever or increasing pain promptly.
- Bleeding (Hemorrhage): Postoperative bleeding can increase intracranial pressure and may require urgent intervention; blood counts and imaging are monitored closely after surgery.
- Swelling (Edema): Brain swelling around the surgical site is common and is often managed with corticosteroids and close monitoring.
- Neurological Deficits: Depending on tumor location and extent of resection, patients may experience temporary or permanent changes in speech, memory, vision, strength, or coordination. Neurorehabilitation can improve function.
- Seizures: Surgery can provoke seizures; anti-seizure medications may be prescribed when indicated.
- Side Effects of Radiation Therapy:
- Acute: Fatigue, headache, nausea, hair loss in the treated area, and scalp irritation. Steroids and supportive care help manage symptoms during treatment.
- Long-term: Some patients develop cognitive changes (memory, concentration), hearing loss, hormonal deficiencies if the pituitary is affected, radiation necrosis, or in rare cases radiation-associated secondary tumors.
- Side Effects of Chemotherapy:
- Common: Nausea, vomiting, fatigue, hair loss, mouth sores, decreased appetite, and lowered blood counts (which increases infection, bleeding, and anemia risk).
- Cognitive effects: Some agents or the combined treatment burden can cause “brain fog” or memory and concentration difficulties; cognitive rehabilitation and supportive therapies can help.
- Targeted Therapy and Immunotherapy: These treatments often have different side-effect profiles — skin reactions, fatigue, GI symptoms, or immune-related events — and require specific monitoring (blood tests, organ function checks).
Practical risk-management tips: ask whether anti-seizure medication or steroids are recommended, ensure regular blood monitoring during chemotherapy, report new neurologic symptoms immediately, and discuss fertility or other long-term concerns before treatment. Questions to ask your team include: What are the most likely complications for my tumor and plan? How will you monitor and manage them? What rehabilitation resources are available?
Your medical team should discuss risks tailored to your diagnosis and propose strategies to reduce harm and support recovery. If you’re considering treatment abroad, confirm local standards for infection control, ICU availability, and postoperative follow-up before committing to care overseas.
How Does the Cost of Brain Cancer Treatment Compare Globally?
The cost of brain cancer treatment varies widely worldwide. Advanced procedures can be very expensive in the USA and Western Europe, which is why many people consider brain tumor surgery cost abroad to reduce expenses while accessing high-quality care.
The financial burden of brain cancer treatment can be substantial, especially for complex procedures like craniotomy, proton therapy, or prolonged courses of chemotherapy. Exact costs depend on tumor type, required therapies, length of stay, and follow-up needs. Medical tourism often provides an alternative route to comparable care at significantly lower prices, but it is important to include travel, accommodation, and post-treatment follow-up when planning your budget.
| Procedure/TreatmentUSA / Western Europe (Est.)Popular Medical Tourism Destinations (Est.)Potential Savings | |||
| Brain Tumor Removal Surgery (Craniotomy) | $50,000 – $150,000+ | $15,000 – $50,000 (e.g., Turkey, India, Mexico) | 50-70% |
| Stereotactic Radiosurgery (e.g., Gamma Knife) | $30,000 – $70,000 | $10,000 – $25,000 (e.g., South Korea, India, Poland) | 60-70% |
| Proton Therapy (Full Course) | $80,000 – $120,000+ | $30,000 – $60,000 (e.g., Czech Republic, South Korea) | 50-60% |
| Chemotherapy (Per Cycle, depending on drug) | $5,000 – $20,000+ | $1,000 – $5,000 (e.g., Thailand, Malaysia) | 70-80% |
*These are estimated costs and can vary significantly based on the specific clinic, doctor’s fees, type of tumor, extent of treatment, length of hospital stay, and individual patient needs. They do not include travel, accommodation, or post-treatment follow-up costs.
When planning care abroad, account for hidden costs (additional imaging, extended stays, medications, and follow-up with your local team). Example: a patient undergoing craniotomy abroad may save 50–70% on the procedure but should budget for travel, a caregiver’s expenses, and follow-up imaging back home. For an accurate estimate, request an all-inclusive quote that lists procedures, surgeon and hospital fees, ICU time, implants (if any), and anticipated follow-up visits.
Why Consider Brain Cancer Treatment Abroad?
Medical tourism for brain cancer can offer meaningful advantages — lower costs, faster access to specialists or specific therapies, and highly personalized care — but it requires careful vetting and planning to ensure continuity and quality.
People choose to seek brain cancer treatment overseas for a mix of practical and clinical reasons. Below are the most common motivators, followed by a balanced look at pros and cons to help you weigh whether international care is right for you or a loved one.
- Cost savings: High-quality brain cancer care in popular medical tourism destinations can cost a fraction of prices in the USA or Western Europe, helping many families afford needed treatment.
- Access to specialized expertise and technology: Some centers offer focused experience in complex neurosurgery, proton therapy, Gamma Knife or clinical trials for novel therapies that may not be accessible locally.
- Shorter wait times: Faster scheduling for urgent procedures can be crucial for aggressive tumors or rapidly worsening symptoms.
- Personalized patient services: Hospitals that serve international patients often provide concierge services, translators, and coordinated packages that reduce logistical burden for the patient and family.
- Second opinions: Traveling for care can double as an opportunity to obtain an independent expert review of your diagnosis and treatment plan.
Pros and cons at a glance:
- Pros: lower procedure costs, potential access to advanced therapy, shorter waits, concierge support.
- Cons: added travel and accommodation costs, need for coordinated follow-up care at home, possible language/cultural differences, and variable regulatory oversight.
Practical recommendations: always verify hospital accreditation and surgeon credentials, ask for an itemized, all-inclusive quote that includes expected follow-up, confirm ICU and emergency capabilities, and plan how you will coordinate post-treatment care with your local medical team. If you balance the clinical benefits, costs, and logistical demands carefully, treatment abroad can be a valuable option in your treatment plan.
Which Countries Offer the Best Value and Quality for Brain Cancer Treatment?
Best countries for brain cancer treatment offering value often combine strong clinical expertise, modern technology (including advanced radiation options), and competitive pricing — examples include Turkey, India, South Korea, Thailand, Germany, and Mexico.
When evaluating top hospitals for brain tumors abroad, consider accreditation, the treating team’s experience with your specific tumor type, and the availability of therapies such as stereotactic radiosurgery or proton therapy. Below are concise country notes plus practical tips for evaluating centers.
- Turkey: Many JCI-accredited hospitals offer high-volume neurosurgery programs, Gamma Knife and advanced microsurgical techniques at competitive prices. Good for people seeking experienced surgical teams and coordinated international patient services.
- India: Long-established medical tourism destination with centers of excellence in neuro-oncology and neurosurgery. India often provides comprehensive care, including complex surgery and follow-up, at much lower cost than Western providers.
- South Korea: Known for cutting-edge technology and specialized centers offering advanced radiation techniques and proton therapy; costs may be higher than some Asian options but still usually below U.S. prices.
- Thailand: Combines strong diagnostic services and patient-centered international care packages; often selected for imaging, initial treatment planning, and streamlined patient logistics.
- Germany: European option with rigorous medical standards and advanced neurological centers; attractive for patients seeking complex diagnostics, specialized second opinions, or therapies grounded in extensive research.
- Mexico: Convenient for North American patients; offers modern facilities and skilled neurosurgeons with the advantage of proximity and lower travel costs.
How to evaluate hospitals in any country: confirm international accreditation (JCI or equivalent), review surgeon and neuro-oncology team credentials and case volumes, ask about availability of specific radiation therapies (stereotactic radiosurgery, proton therapy), check infection and ICU standards, and read independent patient reviews. Also confirm language support, travel accessibility, estimated timeline (including typical wait times), and clear plans for follow-up care once you return home.
Finally, consider logistics for children separately — pediatric neuro-oncology care is highly specialized, and families should seek centers with dedicated pediatric programs. Regardless of country, coordinate with your local medical team before and after overseas care to ensure continuity and the best possible outcomes.
What to Expect When Traveling Abroad for Brain Cancer Treatment?
Planning brain cancer treatment abroad involves coordinating travel, accommodation, visas, and medical records. Expect dedicated medical tourism facilitators who assist with logistics, from airport pick-up to hospital appointments.
Medical travel for a brain tumor requires careful preparation. The process typically follows several steps — initial remote review, travel planning, arrival and pre-treatment workup, the treatment itself, and recovery with coordinated follow-up. Below is a practical guide to what you should expect and how to prepare.
- Initial consultation & planning: Share your key medical records (MRI scans, pathology reports, operation notes, and medication list) for a remote review. Ask for a written treatment plan, estimated timeline, and itemized cost estimate before committing.
- Logistics and documentation: Arrange flights, accommodation, visas, and travel insurance that covers medical evacuation if needed. Confirm the hospital’s international patient services, translator availability, and whether a caregiver can stay nearby.
- Arrival and pre-treatment workup: On arrival you may undergo repeat imaging and consultations to confirm the diagnosis and finalize the plan. Expect local blood tests and possible multidisciplinary team review to adapt the treatment to current findings.
- Treatment phase: The hospital stay varies by procedure — stereotactic radiosurgery may be outpatient or short-stay, while craniotomy often requires several days of inpatient care and ICU monitoring. Confirm anticipated length of stay and postoperative needs in advance.
- Recovery and return planning: Hospitals will provide discharge instructions and a follow-up schedule. Do not book immediate long-haul flights without medical clearance — many surgeons recommend waiting several weeks depending on the procedure and your recovery. Coordinate follow-up imaging and care with your local healthcare team before you travel home.
- Language, culture, and support: Most international centers serving medical tourists provide English-speaking staff and patient coordinators. Still, prepare for cultural differences and confirm communication channels with your treating team.
Pre-travel checklist (brief): bring original and digital copies of MRI scans and pathology, current medication list, a letter from your local doctor, travel and medical insurance details, and contact information for your local neurologist or oncologist. Discuss thrombosis prevention and timing of flights with your team — long flights soon after major surgery carry risks like deep vein thrombosis and may require precautions.
Working with a reputable medical tourism facilitator or the hospital’s international patient office can streamline arrangements and help ensure continuity of care. Before finalizing plans, confirm accreditation, ICU and emergency capabilities, the availability of postoperative rehabilitation, and a clear, written plan for follow-up care once you return home.
How Can I Ensure Safety and Quality When Choosing Brain Cancer Treatment Abroad?
To ensure safe brain tumor treatment abroad, choose internationally accredited hospitals, verify surgeon credentials and experience, get transparent pricing, and work with reputable medical tourism facilitators who vet clinics and support patients through the process.
Safety and quality should be the top priorities when considering treatment overseas. Lower costs are attractive, but they must be balanced against clinical standards, postoperative care, and continuity with your local medical team. Use the checklist below to evaluate providers and protect your health and investment.
- Accreditation: Confirm hospital accreditation (Joint Commission International — JCI — or equivalent). Accreditation indicates adherence to international patient safety and quality standards.
- Surgeon and team credentials: Request the neurosurgeon’s CV, board certifications, fellowship training, and case volumes for your specific tumor type. Ask how many similar procedures they perform annually and for outcomes or complication rates.
- Technology and facility capabilities: Ensure the center has advanced imaging (high-resolution MRI), intraoperative navigation, ICU and blood/blood-product availability, and modern radiation therapy options if needed (stereotactic radiosurgery, proton therapy).
- Transparent pricing and documentation: Get a detailed, all-inclusive written quote covering surgeon and hospital fees, ICU time, implants, pathology, expected length of stay, and planned follow-up visits. Ask about refund or change policies if the plan changes.
- Patient outcomes and reviews: Look for published case series, peer-reviewed outcomes, and independent patient reviews. Request anonymized aggregate outcome data when possible to understand survival and complication rates for your diagnosis.
- Continuity of care and legal/medical record transfer: Confirm how medical records will be transferred to your local team, who will manage follow-up imaging, and what legal protections or malpractice recourse exist. Ensure discharge summaries and contact details for your treating clinicians are provided.
- Reputable facilitators and communication: If you use a medical tourism facilitator, verify their track record and independence. Ensure clear communication channels with translators as needed and that the hospital provides a dedicated international patient coordinator.
If considering experimental options or clinical trials, verify the trial’s registration, Institutional Review Board (IRB) oversight, and published safety data. When in doubt, request a second opinion from an independent academic center. Prioritizing these safety checks will help you access high-quality brain cancer therapy abroad while minimizing risks.
What Are Patient Success Stories from Brain Cancer Treatment Abroad?
Brain cancer survivor stories from medical tourism show people who accessed specialized care, regained function, and in some cases achieved extended survival after receiving advanced treatments at international centers.
While individual stories can be inspiring, they are anecdotal and do not guarantee similar results for everyone. Outcomes depend on tumor type (for example gliomas versus meningiomas), grade, molecular markers, and the timeliness and combination of treatments. That said, many patients report meaningful improvements in symptoms and quality of life after seeking care abroad.
Examples (anonymized): ‘Maria’ from Canada pursued a timely surgical resection and follow-up radiation for a high-grade glioma at an international center when long domestic wait times threatened timely care. After surgery and adjuvant therapy, she experienced symptom relief and was able to continue rehabilitation at home.
‘John’ from the UK traveled to receive specialized proton therapy for a recurrent tumor when it was not available or affordable at home. He completed a full course with manageable side effects and returned to his family with a favorable short-term response. These cases illustrate how accessing specific modalities abroad can expand treatment options for some patients.
Common themes in successful stories include:
- Overcoming financial barriers to access essential care that otherwise would have been unaffordable.
- Finding specialized expertise for complex or rare tumor types (for example certain gliomas) that improved the treatment plan.
- Receiving coordinated, patient-centered support that helped families navigate care, travel, and recovery.
- Achieving improved symptom control and, in some cases, extended survival and better quality of life after multimodal therapy.
How to verify and use patient stories responsibly: ask the hospital for aggregated outcome data or peer-reviewed publications, request anonymized case series for your tumor type, and consult independent review sites and patient advocacy groups. Always treat survivor stories as one piece of information and weigh them alongside clinical data, surgeon experience, and objective outcome measures.
If you find a compelling patient testimonial, ask the provider for references or for outcome statistics for similar cases. Discuss these data with your multidisciplinary team and family to decide whether pursuing care abroad aligns with your goals and gives the best chance of improved survival and quality of life.
Take the Next Step with DGS Healthcare
Ready to explore accredited treatment options for brain cancer abroad? Get a free, no‑obligation quote that compares top clinics, surgeon credentials, and expected costs — with confidential support to help you plan travel, treatment, and follow-up care.
- Compare costs and treatment options across accredited hospitals
- Review surgeon experience and facility capabilities
- Coordinate logistics, visas, and post‑treatment follow‑up
Before you proceed, remember to plan for continuity of care at home, confirm insurance and legal considerations, and ask for detailed, itemized quotes that include anticipated follow‑up visits and imaging.
