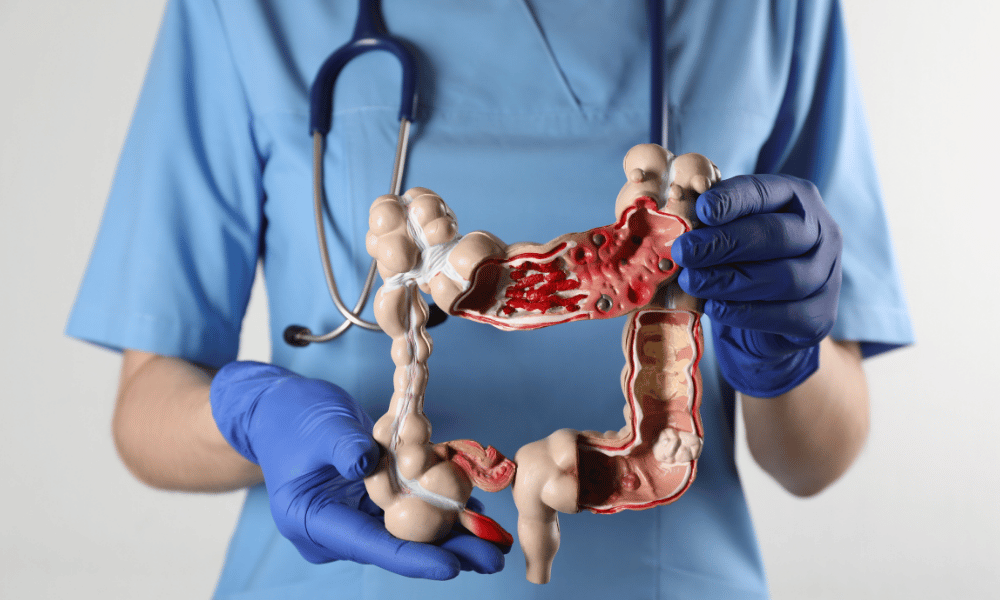
Colon Cancer
A diagnosis of colon cancer can be frightening — but there are effective options. Treatment commonly includes surgery, chemotherapy, radiation, and targeted therapies, chosen based on the cancer’s stage and specific characteristics. Many patients also consider seeking care abroad to access internationally accredited facilities, advanced technology, or shorter wait times; comparative studies and medical tourism reports often show notable cost differences for equivalent care (see sources in the full guide).
Navigating Colon Cancer: Understanding Your Treatment Options Globally
A diagnosis of colon cancer is stressful and raises immediate questions about prognosis, treatment, and next steps. The colon is part of the large intestine, and thanks to advances in medicine, a wide range of effective options exists — from minimally invasive surgery to targeted drugs and immunotherapy for selected tumors.
Why this guide matters: colorectal cancer is one of the most common cancers worldwide, but early detection and modern treatment substantially improve outcomes. This guide provides clear, practical information about:
- Common symptoms and screening (when to get a colonoscopy)
- Causes, risk factors, and genetic considerations
- Standard and advanced treatment options and how they depend on stage
- What to expect if you choose treatment abroad — logistics, safety checks, and costs
Read on for practical information that can help you discuss options with your care team, compare local and international treatment pathways, and decide whether seeking care overseas is right for you. (Note: some immunotherapies are most effective for cancers with specific genetic features, such as MSI‑High/dMMR — details below.)
What are the common symptoms of colon cancer that I should watch for?
Key warning signs include persistent changes in bowel habits, blood in the stool, unexplained weight loss, and ongoing abdominal discomfort. Early detection through screening greatly improves outcomes.
Colon cancer may develop slowly and can be symptom‑free in early stages, which is why regular screening such as colonoscopy is so important. If symptoms appear or persist, prompt medical evaluation helps earlier diagnosis and more effective treatment.
- Changes in bowel habits: Persistent diarrhea, constipation, or a change in stool consistency lasting more than a few days.
- Blood in the stool or rectal bleeding: Bright red blood or dark, tarry stools — while hemorrhoids are common, blood should always be evaluated to rule out more serious causes.
- Persistent abdominal discomfort: Ongoing cramps, gas, bloating, or a feeling of fullness.
- Feeling that the bowel does not empty completely: A continual urge to have a bowel movement even after going.
- Unexplained weight loss: Losing weight without trying can be a warning sign for colon cancer and other cancers.
- Fatigue or weakness: Chronic blood loss from the colon can cause iron deficiency anemia, leading to persistent tiredness and paleness.
When to seek immediate care: If you experience heavy rectal bleeding, severe abdominal pain, signs of bowel obstruction (no bowel movements, vomiting, severe distension), or sudden fainting, seek emergency care right away.
Quick checklist — see a doctor if you have:
- Blood in stool or unexplained weight loss
- New, persistent change in bowel habits >2 weeks
- Unexplained fatigue or symptoms that worry you
If you are over age 45 (or younger with a family history of colon polyps or colon cancer), discuss screening and the timing of a colonoscopy with your healthcare provider. Early screening and removal of polyps can prevent colon cancer and lead to earlier, more treatable diagnoses.
What causes colon cancer and who is most at risk?
Colon cancer most often develops from abnormal cell growth in the lining of the large intestine, frequently arising from benign polyps that can become cancerous over time. A mix of genetic and lifestyle risk factors — and increasing age — influence who is most likely to develop the disease.
Colon cancer begins when cells in the colon start to grow uncontrollably. Many cancers start as small, noncancerous polyps; removing polyps during screening can prevent cancer. Several risk factors change a person’s likelihood of developing colon cancer — some you can modify, others you cannot.
- Age and screening: Risk rises with age. Current guidelines in many countries now recommend beginning screening around age 45–50, but earlier screening is advised for those with risk factors.
- Family history and inherited syndromes: A close relative with colon cancer or polyps increases risk. Hereditary conditions such as Familial Adenomatous Polyposis (FAP) and Lynch syndrome (hereditary nonpolyposis colorectal cancer) confer very high lifetime risk and usually require earlier, more intensive surveillance.
- Inflammatory bowel disease (IBD): Chronic conditions that inflame the colon lining, like ulcerative colitis and Crohn’s disease, raise the risk of dysplasia and cancer over time.
- Polyps and cellular changes: Adenomatous polyps and other abnormal growths of colon cells are precursors to many colon cancers — regular surveillance and removal reduce progression risk.
- Lifestyle factors: Diets low in fiber and high in red or processed meat, physical inactivity, obesity, heavy alcohol use, and smoking are associated with higher risk.
- Medical conditions and treatments: Type 2 diabetes and insulin resistance are linked with increased risk, and prior radiation to the abdomen can raise lifetime risk in some patients.
Understanding your personal risk profile — family history, prior polyps, IBD, and lifestyle — helps determine the best screening schedule and preventative measures. If you have a strong family history or known genetic syndrome, discuss earlier and more frequent surveillance with your doctor or genetic counselor.
Simple steps to lower risk
- Get screened on schedule (colonoscopy removes polyps and aids early diagnosis)
- Increase fiber intake, reduce red/processed meat, and maintain a healthy weight
- Stay physically active, limit alcohol, and stop smoking
- If you have a family history, ask about genetic testing for familial adenomatous polyposis or Lynch syndrome
What types of colon cancer treatments are available today?
Modern colon cancer treatment is personalized and often delivered by a multidisciplinary team. Common options include surgery (open or minimally invasive), chemotherapy, radiation therapy in select cases, targeted drug therapies based on tumor biology, and immunotherapy for specific tumor types.
The choice of treatment depends on the cancer’s stage, location in the colon or rectum, the patient’s overall health, and molecular features of the tumor. Below is a practical summary of the main modalities, typical goals, and when they are commonly used.
Main treatment options and when they’re used
- Surgery (curative intent for many early-stage cancers): Removal of the cancerous part of the colon (colectomy) and nearby lymph nodes is often the primary curative treatment. Options include:
- Polypectomy: Removal of polyps during colonoscopy — may be sufficient for very early lesions.
- Colectomy (open, laparoscopic, or robotic): Resection of the affected colon segment with lymph node sampling to assess stage and reduce cancer spread; minimally invasive approaches often reduce hospital stay and speed recovery.
- Ostomy: Temporary or permanent colostomy/ileostomy may be needed in some cases to protect a surgical join or when reconstruction isn’t possible.
- Chemotherapy (adjuvant, neoadjuvant, or palliative): Uses systemic drugs to kill cancer cells. Common strategies include adjuvant chemotherapy after surgery to reduce recurrence, neoadjuvant chemotherapy to shrink tumors before surgery in some cases, or chemotherapy to control advanced disease and relieve symptoms.
- Radiation Therapy (select use): Radiation is more commonly used for rectal cancer than colon cancer but can be applied to control symptoms, shrink tumors preoperatively in certain cases, or treat localized recurrences.
- Targeted Drug Therapy: Drugs that attack specific abnormalities in cancer cells (for example, therapies against VEGF or EGFR pathways) can be effective in selected patients and often have different side-effect profiles than traditional chemotherapy. Molecular testing guides use.
- Immunotherapy: Activates the immune system to attack cancer cells. It is particularly effective for tumors with certain genetic features (e.g., MSI‑High or deficient mismatch repair — dMMR) and may be used in advanced disease or in clinical trials.
How stage and tumor biology influence choices
Early-stage tumors confined to the colon are often treated with surgery alone. If cancer has spread to lymph nodes or beyond (higher stage), adjuvant chemotherapy is commonly recommended. Advanced disease management frequently combines chemotherapy, targeted agents, and — for appropriate molecular profiles — immunotherapy. Talk with your oncology team about genomic testing to identify targeted drug and immunotherapy options.
Practical notes
- Discuss stage-specific goals with your team: curative vs. control/palliative.
- Ask whether minimally invasive (laparoscopic/robotic) surgery is an option — it can shorten recovery.
- Request molecular profiling (tumor genetic testing) to determine eligibility for targeted therapy or immunotherapy.
- Consider asking about clinical trials if standard options are limited.
Many international cancer centers offer coordinated, multidisciplinary care that can include surgical oncology, medical oncology (chemotherapy and targeted agents), radiation oncology, genetic counseling, and supportive services to manage side effects and improve outcomes.
Who is eligible for colon cancer treatment abroad?
Patients may consider colon cancer treatment abroad when they seek high-quality care, access to advanced procedures or clinical trials, shorter wait times, or more affordable options. Eligibility depends on the patient’s overall health, the cancer’s stage, and practical ability to travel and follow post-treatment care.
Medical travel for colorectal cancer treatment can be a good option for many people, but it’s not right for everyone. Below are common reasons patients explore international treatment and practical factors that influence eligibility.
- Seeking cost-effective care: Patients from countries with high healthcare costs sometimes find comparable care abroad at lower prices, making treatment more accessible.
- Facing long wait times at home: When delays for specialist visits or surgery are long, traveling can provide faster access to necessary treatment — an important consideration for cancer care.
- Needing advanced or specific treatments: Some international centers offer specialized surgical techniques (robotic or minimally invasive), genomic-guided targeted therapies, or clinical trials not available locally.
- Privacy or preference: Some patients value the anonymity and focused attention of receiving care away from home.
- Health and fitness for travel: You must be medically stable enough to travel; many providers require a recent medical evaluation and clearance before accepting international patients.
- Cancer stage and complexity: Early-stage colon cancer patients are often good candidates for travel, while some centers will accept more advanced cases — but very unstable or critically ill patients may be better treated locally.
- Support and logistics: Having family or a caregiver who can accompany you, or a reliable plan for home support, improves suitability for treatment abroad.
Quick self-check: Is travel right for you?
- Can you get medical clearance to travel?
- Is someone able to accompany or support you during recovery?
- Do you need a procedure or clinical trial not available locally?
Recommended pre-travel steps: compile recent medical records (diagnosis, pathology, imaging), get a fitness-for-travel assessment, and request a detailed, all-inclusive treatment quote. A reputable medical tourism facilitator or your care team can help assess eligibility and coordinate logistics for treatment and follow-up.
What is the typical recovery time after colon cancer surgery?
Recovery after colon cancer surgery varies widely — from a few weeks to several months — and depends on the type of operation (open vs. minimally invasive), the cancer’s stage, and your overall health. Typical hospital stays are often 3–7 days, followed by a gradual return to daily activities and any additional treatments recommended by your oncology team.
Every patient’s recovery is unique. Factors such as whether lymph nodes were removed, whether an ostomy was created, and whether you’ll need adjuvant chemotherapy or radiation influence the timeline. Below is a practical, stage-aware outline of what to expect and tips for planning, including for international patients.
- Immediate post-operative period (hospital stay):
- Most patients remain in hospital about 3–7 days after a colectomy; minimally invasive (laparoscopic or robotic) approaches often shorten this stay.
- Early mobilization, pain control, and progressive diet (clear liquids → solids) are priorities to reduce complications and restore bowel function.
- If lymph nodes were removed during surgery, pathology results (which influence staging) may take several days to a few weeks to finalize.
- First few weeks at home:
- Fatigue is common — rest and gradual increases in light activity are recommended. Avoid heavy lifting and strenuous exercise for about 4–6 weeks to allow internal healing and reduce hernia risk.
- Bowel habits may change (diarrhea, constipation) while the intestine adapts; your team will advise dietary adjustments and medications as needed.
- If you have an ostomy, expect training and ongoing support to manage appliances and skin care.
- Long-term recovery and follow-up:
- Many people feel substantially better by 2–3 months, but full recovery can take several months, especially if adjuvant chemotherapy or radiation is given.
- Regular follow-up appointments monitor healing, manage side effects, review pathology/staging (including lymph nodes), and schedule surveillance such as periodic colonoscopy.
Practical advice for patients — especially those traveling for care
- Plan to stay near the treatment center for at least 1–2 weeks after discharge (longer if advised) before flying home; follow your surgeon’s specific guidance about safe travel timing.
- Arrange a follow-up plan with both the international team and your local care team to ensure continuity of care.
- Know warning signs that require urgent attention: fever, increasing abdominal pain, persistent vomiting, inability to pass stool/gas, heavy bleeding, or signs of wound infection — seek immediate care if these occur.
Discuss expected timelines and return-to-work plans with your oncology and surgical team before treatment so you can schedule travel and home support appropriately. Your care team will tailor recovery guidance to your stage, overall health, and treatment plan.
What are the potential risks and side effects of colon cancer treatment?
Treatments for colon cancer can be highly effective but carry risks. Surgery, chemotherapy, and radiation each have specific complications, and newer targeted drugs and immunotherapy have distinct side-effect profiles; your medical team will review expected risks and ways to manage them.
Understanding likely side effects and how they are managed helps patients prepare, reduces anxiety, and improves outcomes. Below is a concise, practical summary of common risks and typical management strategies, plus clear guidance on when to contact your care team.
- Risks and complications of surgery:
- Bleeding: Intraoperative or postoperative bleeding may require transfusion or reoperation; blood loss is monitored closely.
- Infection: Surgical-site or intra-abdominal infections are possible; preventive antibiotics and wound care reduce risk, and infections are treated promptly.
- Anastomotic leak: A serious complication where a surgical join leaks; signs include fever, abdominal pain, or sepsis and require urgent care.
- Bowel obstruction and adhesions: Scar tissue can cause blockage; some cases need medical management or further surgery.
- Ostomy-related issues: If a colostomy/ileostomy is created, skin irritation, leakage, or appliance problems can occur and are managed with training and specialist stoma care.
- Common side effects of chemotherapy:
- Nausea and vomiting: Preventable or controllable with modern antiemetics.
- Fatigue: Very common; activity pacing and supportive care help.
- Changes in bowel habits: Diarrhea or constipation may occur; dietary changes and medications are used.
- Neuropathy: Nerve damage (numbness/tingling) is associated with certain drugs and may be long-lasting; dose adjustments and symptomatic treatments can help.
- Increased infection risk: Lowered white blood cell counts may require growth-factor support or antibiotics.
- Side effects of radiation therapy:
- Skin irritation and local soreness: Typically managed with topical care and supportive measures.
- Fatigue and bowel changes: Diarrhea and discomfort can occur when abdominal or pelvic areas are treated.
- Urinary symptoms: When pelvic tissues are irradiated, frequency or discomfort may occur.
- Targeted therapy and immunotherapy considerations: Targeted drugs can cause specific effects (skin rash, hypertension, hand‑foot changes) depending on the pathway targeted. Immunotherapy can prompt immune-related adverse events where the immune system attacks healthy organs (e.g., colitis, pneumonitis, hepatitis); these are managed with immunosuppressive medications when identified early.
How side effects are managed: your care team will use preventive medications (antiemetics, growth factors), supportive treatments (pain control, nutritional support), and dose adjustments or treatment breaks as needed. Multidisciplinary supportive care teams help maintain quality of life during treatment.
When to contact your doctor or seek urgent care
- Fever or signs of infection (temperature >100.4°F / 38°C)
- Severe, worsening abdominal pain or persistent vomiting
- Inability to pass stool or gas (possible obstruction)
- Heavy bleeding from the rectum or wound
- Sudden breathlessness or chest pain
Open communication with both your local and international care teams is essential to identify and treat side effects promptly. Before traveling for care, ask how side effects will be monitored, who to contact in an emergency, and what supportive services are available during and after treatment.
How does the cost of colon cancer treatment vary worldwide?
The cost of colon cancer treatment varies widely across countries. Medical tourism destinations can offer substantial savings — often a fraction of Western prices — but exact figures depend on the procedure, cancer stage, hospital choice, and length of stay.
Cost is a major reason people consider treatment abroad. Complex care like colectomy plus chemotherapy can be expensive in the United States and some Western countries; many patients find that equivalent or advanced cancer care in other nations is more affordable. Below is a snapshot of estimated price ranges to help you compare and to guide questions when requesting an all‑inclusive quote.
Estimated Cost Comparison Table for Colon Cancer Treatment (Colectomy with Chemo)
| CountryEstimated Cost Range (USD)Notes | ||
| United States | $50,000 – $150,000+ | Highly variable; depends on hospital, stage, surgeon, and insurance coverage. |
| United Kingdom (Private) | $30,000 – $80,000+ | Private care; faster access or treatments not covered by public systems. |
| India | $8,000 – $25,000 | Known for experienced surgeons and advanced cancer centers at lower prices. |
| Mexico | $10,000 – $30,000 | Proximity to North America and competitive pricing in major centers. |
| Turkey | $12,000 – $35,000 | Emerging hub with modern facilities and international patient services. |
| Thailand | $10,000 – $30,000 | Accredited hospitals and comprehensive international packages are common. |
*Estimates are approximate and can change over time. Figures are illustrative and may vary by hospital, surgeon, stage of disease, included services, and year — always request a dated, itemized, all‑inclusive quote.
What to confirm in an all‑inclusive quote
- Exactly which procedures, tests, and medications are included (surgery, anesthesia, pathology, imaging, initial chemo cycles)
- Hospital stay length, surgeon and facility fees, and any implant or device costs
- Pre‑ and post‑operative care, follow‑up visits, and emergency care policy
- Travel‑related costs that may or may not be included (accommodation, airport transfer)
- Validity period of the quote and refund/cancellation policies
Savings from international treatment can make otherwise unaffordable cancer care accessible, but verify credentials, outcomes, and what is included. Ask for recent references, accreditation details, and a clear timeline so you can compare options safely and accurately.
Why should I consider colon cancer treatment abroad?
Seeking colon cancer care abroad can offer meaningful advantages — from lower out-of-pocket costs and shorter wait times to access to advanced technology and specialist teams — but it’s important to weigh benefits against practical and clinical considerations.
Deciding to travel for treatment is a significant choice. For many people, the potential gains (faster scheduling, access to specific procedures or clinical trials, and competitive pricing) make it worth exploring. Below are common reasons patients consider international options, followed by a short due‑diligence checklist and a balanced note on risks to consider.
- Potential cost savings: Many people report substantially lower total bills abroad for comparable colon cancer treatment, which can make otherwise unaffordable care accessible.
- Access to advanced techniques and technologies: Some international centers offer robotic surgery, advanced imaging, or molecular-guided targeted therapies and immunotherapies that may not be readily available locally.
- Shorter wait times: Faster access to diagnostics, specialist consultations, or surgery can be critical in colorectal cancer management where delays may affect outcomes.
- Experienced multidisciplinary teams: International hospitals often assemble coordinated teams (surgical oncology, medical oncology, radiation oncology, genetic counseling) that deliver comprehensive care.
- Improved patient experience: Facilities serving international patients tend to emphasize personalized service, language support, and clear care coordination.
Due‑diligence checklist
- Confirm international accreditation and surgeon credentials (ask for CVs and outcome data).
- Request a dated, itemized, all‑inclusive quote covering pre/post‑op care, pathology, and initial chemo cycles.
- Ask about experience with the specific stage and type of colon cancer you have, including colorectal cancer cases with similar complexity.
- Clarify follow‑up care plans and how your international team will coordinate with your local care providers.
Balanced perspective — risks to keep in mind: Travel and cross‑border care bring logistic and continuity challenges (insurance, legal recourse, and post‑operative follow‑up). Very advanced or unstable patients may be safer treated locally. Discuss potential benefits and limitations with your care team and a trusted facilitator so you can make an informed choice that fits your medical needs and personal situation.
Which countries offer the best value and quality for colon cancer treatment?
Several countries combine experienced oncology teams, modern hospitals, and competitive pricing, making them popular destinations for colon cancer care. When comparing options, prioritize accreditation, surgeon experience, and verified patient outcomes in addition to cost.
Medical travelers commonly choose destinations that offer a balance of high-quality care and value. Below are countries frequently selected for colorectal cancer treatment and what they typically offer.
- India: Many hospitals have JCI accreditation and multidisciplinary cancer teams. India is known for experienced surgical oncology teams, advanced diagnostic capabilities, and relatively low overall treatment costs.
- Mexico: A convenient option for North American patients due to proximity and shorter travel times; several centers provide English-speaking staff, modern facilities, and competitive pricing for colon and rectal cancer care.
- Turkey: Offers modern hospitals with international accreditation and experienced surgical teams; centers often emphasize patient comfort and coordinated care for international patients.
- Thailand: Known for excellent patient experience and comprehensive packages that can include accommodation and transfers; many Bangkok hospitals provide advanced oncology services and international patient support.
- South Korea: A leader in medical technology and research, offering advanced diagnostics, robotic surgery options, and strong integration of research and clinical care — often chosen when cutting-edge diagnostics or surgical techniques are priorities.
- Malaysia: Provides English-speaking medical professionals, JCI‑accredited hospitals in major cities, and patient-focused packages with an emphasis on comfort and coordinated international care.
How to choose a hospital and team
- Check international accreditation (e.g., JCI) and recent accreditation status.
- Verify surgeon and oncology team credentials, experience with colon/rectal cancer, and case volumes.
- Request outcome data or patient references for similar stages and treatments.
- Confirm language support, international patient coordinators, and post‑op follow‑up arrangements with local providers.
- Ask about timelines, clinical trial availability, and whether molecular testing or genomic-guided treatment is available.
When comparing countries and centers, balance cost with demonstrated quality and the ability of the team to treat your specific stage and type of colorectal cancer. A well‑coordinated team and clear follow‑up plan are as important as the initial procedure.
What should I expect when traveling for colon cancer treatment overseas?
Expect a structured process that begins with a medical review and virtual consultation, continues through travel planning and arrival at a JCI‑accredited or equivalent facility, and includes the treatment episode plus coordinated post‑operative care and follow‑up. Many centers assign an international patient coordinator to help manage logistics and communication with your local care team.
Traveling for colorectal cancer care requires careful planning. The typical steps below will help you prepare and know what to expect at each stage.
- Initial medical review and consultation:
- You will send your medical records (diagnosis, pathology reports, colonoscopy findings, imaging scans) for review; include recent test dates and reports to speed diagnosis clarification.
- An international patient coordinator or the hospital team will provide a proposed treatment plan, estimated timeline, and a dated, itemized cost estimate.
- A virtual consultation with the treating specialist is usually arranged so you can ask questions and confirm the plan before committing to travel.
- Travel logistics and preparation:
- Arrange passports, visas (some countries have medical visa options — check embassy guidance), flights, and accommodation near the hospital; many hospitals offer international patient services or partner hotels.
- Obtain travel insurance that explicitly covers medical complications or extended stays; confirm coverage limits and emergency evacuation policies if relevant.
- Bring an up‑to‑date list of medications, allergies, and contact details for your local care team to facilitate continuity of care.
- Arrival and pre‑treatment assessment:
- You’ll usually be greeted by a hospital representative. Expect pre‑operative tests (blood work, updated imaging) and consultations with surgery and anesthesia teams to confirm the plan and consent.
- Use this time to clarify post‑op care, expected hospital length of stay, and how follow‑up will be coordinated with your local doctor.
- Treatment and in‑country recovery:
- Undergo planned procedures (surgery, chemotherapy, radiation as indicated). Expect a hospital stay per the surgeon’s guidance (often 3–7 days for colectomy) followed by monitored recovery in nearby accommodation for initial follow‑up or first chemo cycles.
- Many centers provide physical therapy, dietary counseling, and stoma care education if needed to support recovery.
- Post‑treatment coordination and return home:
- Before departure you should receive a comprehensive medical report, pathology results (when available), medication lists, and clear instructions for follow‑up care.
- Arrange handover communication between the international team and your local oncology/surgical team to ensure continuity of surveillance and any further treatment.
- Plan your travel home timing according to medical advice — surgeons often recommend staying locally for a minimum period (commonly 1–2 weeks or longer depending on the procedure) before flying.
Practical checklist — what to send and ask for
- Copies of pathology reports, colonoscopy findings, and imaging (CT/MRI/PET) — digital files preferred
- List of current medications and allergies, plus recent lab results
- Itemized, dated treatment quote that lists what is included (surgery, anesthesia, pathology, initial chemo cycles, hospital stay)
- Clear plan for post‑op follow‑up, including who will coordinate with your local team
- Advice on minimum recommended stay after surgery before flying home
Working with a reputable facilitator or the hospital’s international patient office can simplify arrangements and reduce uncertainty. Always verify accreditation, surgeon credentials, and references, and confirm insurance and emergency procedures before you travel.
How can I ensure safety and quality when getting colon cancer treatment abroad?
Protect your health by choosing accredited hospitals, verifying surgeon and oncology team credentials, checking patient outcomes, and confirming transparent pricing and emergency protocols. A careful review and clear communication reduce risk and help ensure high-quality colon cancer care overseas.
Due diligence is essential when pursuing cancer treatment abroad. Below are practical steps, questions to ask, and items to request so you can evaluate safety, quality, and continuity of care.
- Check international accreditation and facility standards: Prioritize hospitals with recognized international accreditation (e.g., Joint Commission International). Verify current accreditation status on the accreditor’s website and confirm the hospital’s oncology program credentials.
- Verify physician and team credentials: Ask for the treating surgeon’s and oncologist’s CVs, board certifications, subspecialty training, and case volume for colon and colorectal cancer. Confirm experience with the specific stage and procedure you need.
- Review outcomes and patient feedback: Request anonymized outcome data (complication rates, 30‑day mortality, recurrence statistics for similar stages) and read independent patient reviews or testimonials. Facilitators may be able to provide references from prior international patients.
- Demand transparency in pricing and scope: Get a dated, itemized, all‑inclusive quote that lists hospital fees, surgeon fees, anesthesia, pathology, imaging, medications, expected length of stay, and whether initial chemotherapy cycles are included. Ask what is excluded (flights, accommodation, extended stays).
- Confirm communication and handover plans: Ensure the team will provide a clear written treatment plan in your language and coordinate transfer of medical records and follow‑up with your local care team after you return home.
- Ask about emergency and post‑operative protocols: Clarify emergency procedures, availability of ICU, blood products, and the hospital’s policy for managing complications in international patients. Know who to contact 24/7.
- Use reputable facilitators and verify their role: If using a medical tourism facilitator, confirm how they vet hospitals and clinicians, what services they provide (logistics, translation, record transfer), and request references. Facilitators can streamline coordination but should not replace your clinical discussions with treating physicians.
Questions to ask a surgeon or oncology team
- How many colon/colorectal cancer cases like mine have you treated in the past year?
- What are your complication and success rates for this procedure and stage?
- Will you provide a written treatment plan and a recovery timeline?
- How will you coordinate with my local care team after I return home?
By taking these steps — checking accreditation, verifying the team, demanding transparent quotes, and confirming follow‑up and emergency plans — you can significantly reduce risk and increase confidence in receiving high-quality colon cancer care abroad. Always keep open lines of communication with both your international and local care teams.
What are patient success stories from colon cancer treatment abroad?
Many people have found timely, high-quality colon cancer care overseas that combined advanced treatment options with lower out-of-pocket costs and coordinated follow-up. The examples below are anonymized summaries meant to illustrate typical scenarios and outcomes reported by international patients.
Patients choose international care for different reasons — reducing wait time, accessing a specific procedure or clinical trial, or making treatment affordable. The following anonymized case summaries highlight common themes: faster access to surgery, use of advanced techniques or molecular-based therapies, and substantial cost savings compared with some Western quotes.
- “Maria’s experience (anonymized)”: A 55‑year‑old with an early-stage colon cancer faced a multi‑month wait locally. After contacting an international center, she underwent a laparoscopic colectomy within weeks. The care team provided clear pre‑op instructions, experienced surgical oncology care, and prompt post‑op support; she recovered quickly and reported lower total costs than private care at home. Takeaway: faster scheduling and minimally invasive surgery can shorten recovery time and reduce overall expense.
- “John’s advanced treatment (anonymized)”: A patient with stage III disease sought genomic profiling and personalized therapy not readily available locally. Through a specialist center, he received molecular testing that guided targeted therapy alongside surgery, resulting in notable tumor regression. Takeaway: tumor profiling can open targeted drug or immunotherapy options that improve outcomes for selected patients.
- “A family’s choice for affordable care (anonymized)”: Facing high out‑of‑pocket costs at home for early‑stage surgery, a family pursued a reputable international hospital with English‑speaking staff and transparent pricing. The surgery was successful, and their overall medical bill was substantially lower than the initial domestic quote. Takeaway: verified centers can provide accessible, high‑quality care at lower cost when transparency and accreditation are confirmed.
Important note: these are anonymized illustrative cases, not guarantees of outcomes. Individual results vary by stage, tumor biology, overall health, and the specific treatments used. Percentages referenced in anecdotal reports (e.g., “70% less”) are approximate and depend on many factors — always request a dated, itemized quote and outcome data when evaluating options.
Quick comparison checklist from these stories
- Timeline: how quickly can the center schedule surgery or the first consultation?
- Clinical match: does the center have experience treating your stage and tumor type?
- Costs/quotes: is the pricing itemized and dated? What exactly is included?
- Continuity: will the center coordinate with your local team for follow‑up?
If you’re considering treatment abroad, ask for anonymized case references, outcome statistics for similar stages, and details about post‑operative support — and make sure all patient stories are used with consent or clearly presented as illustrative examples.
Take the Next Step with DGS Healthcare
Ready to explore treatment options abroad? Discover top clinics, compare prices, and get a free, no‑obligation quote tailored to your needs with DGS Healthcare. Quotes are confidential and typically include a preliminary treatment plan, estimated costs, and an expected timeline.
Need help now? International patient coordinators are available to assist with questions about care, travel planning, and coordination with your local team.
