Conformal Radiation Therapy
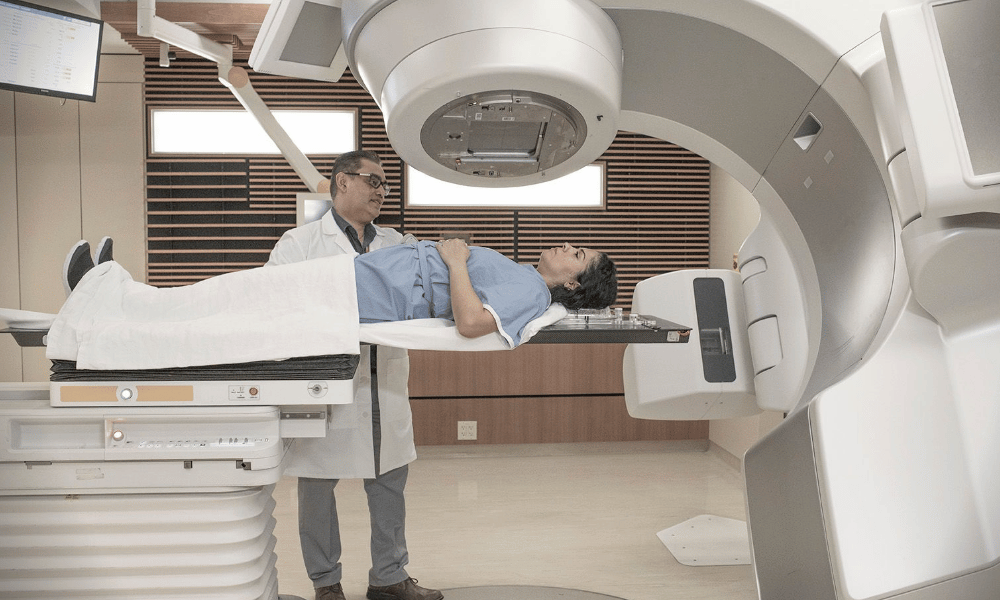
Conformal Radiation Therapy (also called 3D‑CRT) is a precise radiation treatment that uses 3D imaging (CT, sometimes MRI or PET) to shape radiation beams so they match the exact contours of a tumor, reducing exposure to surrounding healthy tissue. This targeted approach aims to improve cancer control and lower side effects compared with older, non‑conformal methods (source: ASTRO/NCCN); below you’ll find who may be a candidate, how the technique works, typical side effects, and cost considerations — plus tips on comparing treatment programs.
Targeting Cancer Precisely: Your Guide to Conformal Radiation Therapy
A cancer diagnosis raises urgent questions about treatment effectiveness and side effects. Conformal Radiation Therapy (CRT or 3D‑CRT) offers a precise radiation treatment option that aims to concentrate radiation on the tumor while protecting nearby organs, helping patients and their care team balance cure and quality of life.
Using advanced 3D imaging (CT and, when needed, MRI or PET), CRT maps the tumor and shapes radiation beams so each beam conforms to the tumor’s contours. The shaped beam approach reduces dose to healthy tissue and allows higher, more effective doses to the cancer (source: ASTRO/NCCN).
CRT is commonly used for many solid tumors — prostate, lung, brain, head and neck, breast, and gastrointestinal cancers — especially when tumors sit close to vital structures. In the sections below you’ll learn who may be a candidate, how the treatment and planning work, expected side effects and recovery, and practical cost and program comparisons to help you discuss options with your oncology team.
Example: a patient with a small prostate tumor may receive a CRT treatment plan that uses multiple shaped beams each day to concentrate dose on the tumor while sparing the rectum and bladder — a typical clinical scenario where conformal radiation is chosen.
What Conditions Does Conformal Radiation Therapy Treat?
Conformal Radiation treats many types of solid tumors by shaping radiation to the tumor’s form so healthy tissue nearby receives less dose.
Conformal Radiation Therapy is a versatile radiation treatment used for a range of solid tumors. Its main value is delivering a high, focused dose to the tumor while sparing adjacent organs. Typical clinical uses include:
- Prostate Cancer (curative/adjuvant): Commonly used to concentrate dose on the prostate and reduce exposure to the rectum and bladder.
- Lung Cancer (early-stage or combined therapy): Useful for localized lung tumors, with special planning to account for breathing motion.
- Brain Tumors (primary and metastases): Precision helps protect critical brain tissue and preserve neurologic function.
- Head & Neck Cancers: Chosen to spare salivary glands, spinal cord, eyes and other sensitive structures.
- Breast Cancer (post‑lumpectomy): Targets the lumpectomy cavity and nearby nodes while reducing dose to heart and lung.
- Gastrointestinal and Pelvic Tumors: Esophageal, rectal, cervical and uterine cancers may use conformal approaches to protect abdominal organs.
Selection depends on tumor size, location and how clearly the tumor shows up on imaging (CT, MRI, or PET). Your oncology team will review scans and create a treatment plan to decide whether conformal radiation is the best option for the specific tumor and area of the body.
What Are the Common Symptoms Requiring Radiation Treatment?
Symptoms that lead to radiation treatment vary by cancer type and location — think persistent pain, new lumps, trouble swallowing, or unexplained weight loss — but those signs always require medical evaluation to determine the right diagnostic scans and treatment plan.
Conformal Radiation Therapy is a treatment, not a diagnostic test. Still, recognizing common warning signs helps you seek timely care. Many symptoms overlap with benign conditions (e.g., infection, inflammation), so persistent or worsening symptoms should prompt a visit with your clinician for appropriate imaging and evaluation.
- Local pain or new lumps: Ongoing pain in a specific area, or a new lump (breast, neck, groin), may indicate a tumor and warrants imaging.
- Changes in function: Difficulty swallowing, persistent hoarseness, or changes in bowel/bladder habits should be evaluated for possible cancers of the head & neck, esophagus, colorectal, or pelvic region.
- Unexplained weight loss or fatigue: Significant weight loss or persistent fatigue may be signs of an underlying cancer or other serious illness.
- Unusual bleeding or skin changes: Blood in stool or urine, abnormal vaginal bleeding, a persistent cough with blood, or a changing mole should prompt immediate medical review.
Next steps: if symptoms persist, your doctor will likely order imaging (CT, MRI or PET) and refer you to a specialist. If a tumor is found, the oncology and radiation care team will discuss whether conformal radiation or another treatment is most appropriate. When in doubt — see a clinician promptly.
What Are the Causes and Risk Factors for Cancers Treated by Conformal Radiation Therapy?
Causes and risk factors for cancers that may be treated with conformal radiation are varied — including genetics, lifestyle choices, infections, environmental exposures, and age — and understanding them helps guide screening and prevention efforts.
Most cancers arise from a mix of inherited and acquired factors. Below are common risk categories to discuss with your care team; for personalized advice, ask your doctor about appropriate screening (CT/MRI/PET scans) and genetic counseling when relevant.
- Lifestyle factors: Smoking/tobacco is a leading cause of lung, head & neck and other cancers; excessive alcohol raises risk for head & neck, liver and breast cancers; poor diet, obesity, and inactivity are linked to colorectal, breast and pancreatic cancers.
- Environmental exposures: Long-term contact with carcinogens such as asbestos or radon, excessive UV radiation, certain industrial chemicals, and air pollution can increase cancer risk in affected tissues.
- Infections: Some viruses and bacteria raise cancer risk (HPV → cervical/head & neck; hepatitis B/C → liver; EBV → nasopharyngeal cancers; H. pylori → stomach cancer).
- Genetic and hereditary factors: A family history or inherited mutations (for example, BRCA1/BRCA2 or Lynch syndrome) can substantially increase risk for specific cancers; consider genetic counseling if family history is concerning.
- Age and chronic conditions: Cancer risk generally rises with age, and long-standing inflammation (e.g., inflammatory bowel disease) can increase risk in the affected body area.
These are general points — talk with your oncology team to understand which risk factors apply to you, how often you should get screening scans, and what lifestyle changes or preventive measures can reduce your personal cancer risk.
How Does Conformal Radiation Therapy (3D CRT) Work?
3D conformal radiation (3D‑CRT) uses detailed imaging to build a 3D map of the tumor and nearby organs so external beam radiation can be shaped to the tumor’s contours, delivering a high, focused dose while sparing healthy tissue.
Conformal Radiation Therapy (commonly called 3D‑CRT) applies modern imaging and computerized planning to tailor each treatment. Below is a clear, step‑by‑step outline of the process (infographic suggestion: Imaging → Planning → Delivery → Verification):
- Imaging & Simulation: The process begins with high‑resolution scans (CT; often fused with MRI or PET) to visualize the tumor and surrounding organs. During simulation you are positioned and sometimes immobilized (molds, masks) so the treatment setup can be precisely reproduced for every session.
- Treatment planning: Radiation oncologists and medical physicists use a treatment planning system (specialized computer software) to contour the target volume and organs at risk, then design multiple shaped beams. Multi‑leaf collimators (MLCs) inside the linear accelerator form each beam’s shape so the dose conforms to the tumor.
- Beam delivery (external beam therapy): On treatment days you lie on the couch while a linear accelerator (linac) rotates and delivers radiation beams from several angles. The combined beams deposit a concentrated dose in the tumor while minimizing dose to healthy tissue; each session is typically brief and painless.
- Verification & monitoring (IGRT): Image‑guided radiation therapy techniques—X‑rays or on‑board CT scans—verify patient and tumor position before and sometimes during sessions to ensure the plan is delivered accurately.
Why not IMRT or SBRT? Intensity‑modulated radiation therapy (IMRT) and VMAT are advanced planning/delivery types that modulate beam intensity for even finer dose shaping; they may be chosen over 3D‑CRT for complex targets. Your radiation team will compare options and create the best treatment plan based on tumor type, location, and the desired balance of dose and side‑effect risk.
Who is an Ideal Candidate for Conformal Radiation Therapy?
Ideal candidates typically have well‑defined solid tumors in locations where precise radiation can spare nearby vital organs; suitability is determined by a multidisciplinary oncology team after imaging and review.
Your care team will evaluate many factors when deciding if conformal radiation is right for you. Common characteristics that make someone a good candidate include:
- Solid, localized tumor: CRT is aimed at solid tumors (not blood cancers) that can be clearly identified on scans.
- Well‑defined on imaging: If the tumor’s borders are visible on CT, MRI, or PET, the radiation planning team can shape beams precisely to the target.
- Location near critical structures: Tumors close to organs such as the spinal cord, heart, lungs, eyes, bladder, or rectum often benefit from CRT’s ability to limit dose to the surrounding tissue.
- Appropriate stage and intent: CRT is frequently used for curative or adjuvant treatment of localized or locally advanced disease and can also be used for palliation when symptom relief is the goal.
- Fit for treatment course: Patients should be well enough to attend daily sessions over the prescribed course (timing and number of sessions vary by tumor and plan).
Typical decision flow: imaging → multidisciplinary review (tumor board) → treatment planning (computerized treatment plan) → delivery. Your radiation oncology team will compare options (for example, CRT vs. IMRT or surgery) and recommend the treatment plan that best balances effectiveness and side‑effect risk for your part of the body.
What is the Recovery Time and What Can I Expect After Treatment?
Recovery from Conformal Radiation Therapy mainly involves managing predictable, usually temporary side effects such as fatigue and localized skin changes; most people see symptoms peak near the end of treatment and then gradually improve over weeks to a few months with appropriate follow‑up care.
Because conformal radiation limits dose to healthy tissue, recovery is often more manageable than older, less targeted approaches. Treatment isn’t surgery — your body heals over time as damaged cells are cleared. Here’s what patients commonly experience and practical steps to manage them.
During and immediately after treatment
- Daily life and sessions: Most people continue routine activities. Each session typically takes about 15–30 minutes, though total clinic time may be longer for setup.
- Fatigue: The most common side effect, often building over weeks and lasting several weeks to months after treatment ends. Prioritize rest, light activity as tolerated, and good nutrition.
- Skin reactions in the treated area: Redness, dryness, itchiness or mild peeling (like a sunburn) can occur; use gentle skin care as advised by your care team and avoid irritants and sun exposure.
- Site‑specific effects: Expect location‑dependent symptoms (e.g., throat soreness and swallowing difficulty for head/neck; cough or mild breathlessness for chest; nausea or bowel changes for abdomen/pelvis). Your team will explain likely effects for your treatment area.
Post‑treatment recovery and follow‑up
- Gradual improvement: Acute side effects usually peak near treatment end and then slowly subside over weeks to months; fatigue often resolves last.
- Follow‑up care and imaging: Regular visits with your oncology team are essential. Imaging scans (timing varies by tumor type — often weeks to months after treatment) check response and guide further care.
- Long‑term effects: Rare but possible (fibrosis, organ function changes, very small increased risk of secondary cancers). Your team tailors the treatment plan to minimize these risks.
- Self‑care and red flags: Rest, hydrate, eat well, and follow skin‑care instructions. Contact your care team promptly for high fever, severe pain, bleeding, sudden shortness of breath, or any rapidly worsening symptoms.
Your radiation oncology team will give a personalized timeline and tips for recovery based on your treatment plan. If you’re comparing programs, ask about expected side effects, the typical time to recovery, and how follow‑up care is coordinated with your local providers.
What Are the Risks and Potential Side Effects of Conformal Radiation Therapy?
Although highly precise, conformal radiation can still cause side effects such as fatigue and localized skin changes; careful treatment planning and modern delivery techniques help reduce dose to healthy tissue and lower the likelihood of severe complications.
Conformal Radiation Therapy is an effective cancer treatment, but like all therapies it carries risks. Side effects depend on the dose, the part of the body treated, and individual sensitivity. They are commonly grouped as acute (during or shortly after treatment) and late (months to years later).
Common acute side effects (weeks to months):
- Fatigue: Very common and often builds over the course of treatment; energy typically improves gradually after the final session.
- Skin reactions in the treated area: Redness, dryness, itching or peeling (similar to a sunburn) are common and usually temporary; follow your care team’s skin‑care advice.
- Hair loss: May occur only in the area that receives radiation; often temporary unless high doses target the scalp or brain.
- Site‑specific effects: Expect location‑dependent symptoms (e.g., sore throat and swallowing difficulty for head/neck; cough for chest; nausea or bowel changes for abdomen/pelvis).
Potential late effects (months to years):
- Fibrosis: Scar tissue can form in the treated part of the body, which may affect organ function (for example, lung fibrosis after chest radiation).
- Organ dysfunction: Depending on the area treated, there is a small risk of long‑term effects (cardiac, pulmonary, neurological, or bowel/bladder changes).
- Secondary cancers: A very rare long‑term risk where radiation contributes to a new cancer in the irradiated field decades later; modern planning aims to minimize this risk.
Your radiation oncology team uses careful treatment planning and customized beam shaping to reduce exposure of healthy tissue and radiation beams to non‑target parts of the body. They will explain expected side effects for your specific treatment plan, give guidance on medications and supportive care, and tell you which symptoms (for example, high fever, severe pain, heavy bleeding, or sudden breathing problems) require immediate contact with the team.
How Much Does Conformal Radiation Therapy Cost Worldwide?
The cost of Conformal Radiation Therapy varies widely by country, clinic, and the complexity of the treatment plan — typical ranges are shown below as estimates to help you compare options and plan your care.
Price is an important factor for many patients, especially when insurance coverage is limited. Costs depend on the type and stage of cancer, the number of fractions (treatment sessions), pre‑treatment imaging and simulation, the sophistication of planning, physician fees, and whether hospitalization or additional procedures are required. For clarity, always ask providers for an itemized program quote that lists what’s included.
The table below offers general, country‑level estimates for conformal radiation (CRT). These are ballpark figures — request a detailed treatment plan and full cost breakdown from any clinic you consider.
| CountryEstimated Cost Range (USD)Notes on Cost Factors | ||
| United States | $30,000 – $100,000+ | Higher costs reflect advanced technology, complex planning, and variable insurance coverage; ask if imaging, planning, and follow‑up are included. |
| United Kingdom | $25,000 – $70,000+ | Private sector pricing varies; check what imaging, planning and physician fees are included in the package. |
| Germany | $20,000 – $60,000+ | Strong medical infrastructure; costs depend on clinic reputation and complexity of the treatment plan. |
| India | $5,000 – $15,000+ | Lower costs with many world‑class centers; confirm included imaging, planning, and follow‑up to compare programs fairly. |
| Mexico | $8,000 – $20,000+ | Popular for cross‑border care; evaluate clinic accreditation and whether the package covers imaging and follow‑ups. |
| Turkey | $7,000 – $18,000+ | Emerging medical tourism destination with modern hospitals; compare treatment plans and included services. |
| Thailand | $6,000 – $16,000+ | Known for quality patient care and hospitality; verify the scope of the program (planning, imaging, follow‑up). |
Before committing, ask for an itemized quote that shows the number and type of sessions, what imaging and planning are included, surgeon/oncologist fees, follow‑up visits, and any expected travel or accommodation costs. That lets you fairly compare programs and choose the best option for your treatment and budget.
Why Should I Consider Conformal Radiation Therapy Abroad?
Patients consider conformal radiation abroad for potential cost savings, access to specialized teams and technology, shorter waits, and personalized program packages — but careful vetting and follow‑up planning are essential.
Traveling for Conformal Radiation Therapy (CRT) can make sense for some patients. Common reasons include:
- Significant cost savings: In many countries the total price for a treatment program — including planning scans and sessions — can be substantially lower, making life‑saving therapy more affordable.
- Access to technology and expertise: Some centers abroad offer advanced machines, experienced radiation oncologists, and dedicated teams that specialize in complex cases.
- Shorter waiting times: Faster scheduling in private international clinics can allow quicker start of treatment — an important factor for time‑sensitive cancers.
- Privacy and patient experience: Many international programs emphasize personalized care, discreet scheduling, patient coordinators, and comfortable accommodations.
If you’re considering treatment abroad, add a short risk/benefit checklist: verify facility accreditation and physician credentials, confirm the detailed treatment plan and what the program includes (imaging, number of sessions, follow‑up), plan how post‑treatment care will be coordinated with your local team, and account for travel, visa and accommodation logistics. Discuss options with your oncology team to ensure continuity of care and safe, effective treatment.
How Can I Ensure Safety and Quality for Radiation Therapy Abroad?
To reduce risk when arranging radiation therapy internationally, prioritize accredited hospitals, verify physician credentials and equipment, request a detailed treatment plan, and confirm how follow‑up care will be handled with your local team.
Traveling for cancer care requires extra due diligence. Use this concise checklist to evaluate safety and quality before committing to a program abroad.
- Check international accreditation: Look for recognized accreditations (for example, JCI) that indicate the facility follows global patient‑safety standards.
- Verify physician and team credentials: Confirm board certification, experience with conformal radiation or IMRT, and ask for CVs or professional affiliations; ensure the center has an experienced multidisciplinary team.
- Review technology and machines: Confirm the clinic uses modern linear accelerators and treatment planning systems (computerized planning, MLCs) suitable for external beam conformal radiation; outdated machines can affect treatment accuracy and tissue sparing.
- Request a detailed treatment plan: Ask for a written treatment plan that lists number of fractions, total dose, imaging used for planning/verification, expected side effects, and how the team monitors delivery and adjusts the plan if needed.
- Confirm follow‑up and continuity of care: Ensure the program explains post‑treatment follow‑up, how records will be shared with your local provider, and who to contact for complications after you return home.
- Read patient reviews and request outcomes: Look for verified testimonials and, where possible, anonymized outcome data for the specific treatment type and tumor site.
- Understand legal, insurance and logistics: Check malpractice and patient‑safety policies, visa/ travel constraints, and whether your insurer will cover any complications or follow‑up at home.
A trustworthy program will provide clear answers to each checklist item and share a transparent treatment plan. If helpful, use a reputable medical tourism facilitator to compare programs, but always independently verify credentials and the specifics of the proposed treatment plan before you travel.
Take the Next Step with DGS Healthcare
Ready to compare conformal radiation treatment options abroad? Discover accredited clinics, compare program details and costs, and get a free, itemized quote tailored to your needs — including follow‑up care coordination and expected side‑effect management.
