Testicular Cancer Treatment
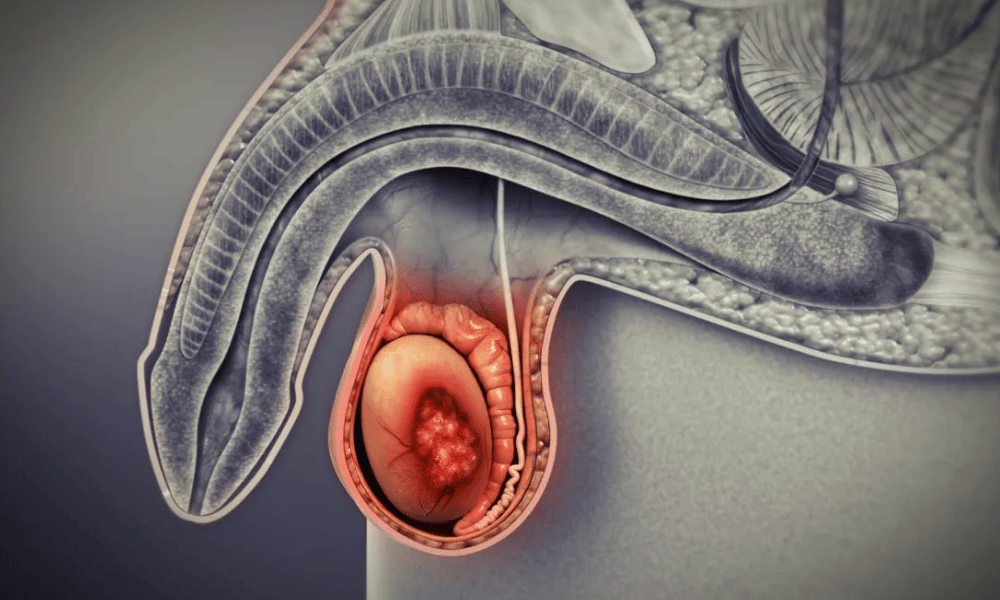
Testicular cancer is highly treatable and most often affects younger men. It commonly appears as a lump or swelling in a testicle; treatment usually begins with surgery (orchiectomy) and may include chemotherapy or radiation, with very good cure rates when detected early.
Navigating Testicular Cancer: Your Guide to Treatment, Recovery, and Global Options
A diagnosis of testicular cancer can be frightening and raise many questions about causes, diagnosis, and treatment. This cancer most often affects men in early adulthood; being informed about early signs, staging, and treatment choices gives you the best chance for a positive outcome. This guide provides clear, practical information about symptoms, causes of testicular cancer, how it’s diagnosed and treated, what recovery looks like, and options for seeking safe, affordable care abroad.
Quickly, here’s what you’ll find in this article:
- How to spot early signs (so you can see a doctor promptly)
- Common causes and risk factors to discuss with your clinician
- How testicular cancer is diagnosed and the main treatment options
- What recovery and long-term follow-up involve
- Practical information about costs and safe medical tourism choices
People often ask, “Can testicular cancer be cured?” In many cases, yes — especially when detected early. If you’re concerned about a lump, swelling, or any change in your testicles or scrotum, see a doctor as soon as possible. Throughout this guide we’ll use plain language and evidence-based information to help you make informed decisions about your care.
What are the Early Symptoms and Signs of Testicular Cancer?
The most common early sign of testicular cancer is a painless lump or swelling in one testicle. Other warning signs include a feeling of heaviness, dull ache in the groin or lower abdomen, or sudden fluid buildup in the scrotum.
Early recognition of symptoms improves the chance of prompt diagnosis and effective treatment. Testicular cancer often produces noticeable changes in the affected testicle rather than vague systemic symptoms. A painless lump or swelling — sometimes described as pea‑ or grape‑sized — is the classic presentation and should prompt a medical review.
Other signs to watch for include:
- Heaviness in the scrotum: a persistent sensation of weight or fullness.
- Dull ache or pain: in the lower abdomen, groin, or testicle.
- Sudden fluid collection (hydrocele): a noticeable swelling from fluid in the scrotum.
- Pain or discomfort: in a testicle or scrotum (though many tumors are painless).
- Breast changes: enlargement or tenderness of the breasts (less common; related to hormone changes from some tumors).
- Back pain: persistent lower back pain can occur if cancer has spread to lymph nodes behind the abdomen.
Many of these symptoms can also be caused by benign conditions such as epididymitis (infection), orchitis, a hydrocele, or a spermatocele. That said, any new lump, swelling, or persistent change in a testicle or scrotum deserves prompt evaluation by a doctor.
How to check your testicles (simple self-exam)
Do a monthly self-exam after a warm bath or shower when the scrotum is relaxed: hold each testicle between thumb and fingers and roll it gently — you’re feeling for any lumps, changes in size, or areas of hardness. It’s normal for one testicle to be slightly larger than the other; the key is to notice new or persistent changes.
When to see a doctor
See a doctor promptly if you discover a lump, swelling, persistent ache, or any other unexplained change in a testicle or scrotum. Don’t wait several weeks — early evaluation leads to earlier diagnosis and a wider range of treatment options. Bring any relevant history (previous testicular problems, undescended testicle) and note how long the change has been present.
What Causes Testicular Cancer and Who is at Risk?
The exact cause of testicular cancer is not fully known. Researchers believe most cases start in germ cells (the cells that make sperm), and several risk factors — such as an undescended testicle, family history, or certain genetic conditions — increase a man’s chance of developing the disease.
While a single definitive cause hasn’t been identified, doctors have found consistent risk factors that raise the likelihood of testicular cancer. Importantly, having one or more risk factors does not mean you will develop cancer, and many men diagnosed have no known risks. Understanding these factors helps you and your doctor decide on appropriate vigilance and follow-up.
Key risk factors include:
- Cryptorchidism (undescended testicle): This is the strongest known risk factor. Men born with one or both testicles that did not descend into the scrotum have a higher lifetime risk of testicular cancer; risk remains elevated even if the testicle is surgically corrected, though early correction may reduce risk.
- Family history: A father or brother with testicular cancer increases your risk compared with men without such family history.
- Previous testicular cancer: Men who had cancer in one testicle are at increased risk of cancer in the remaining testicle.
- Age and demographics: Testicular cancer most often affects younger men, particularly those between late teens and their 30s. Incidence varies by race and ethnicity, with higher rates generally reported in White men in many countries.
- Genetic conditions: Certain genetic syndromes (for example, Klinefelter syndrome) are associated with increased risk.
- Immune status: Some research suggests men with HIV may have a modestly higher risk, though findings vary across studies.
Unlike many other cancers, lifestyle factors such as diet, exercise, or smoking have not been clearly linked to testicular cancer. The leading theory is that the cancer develops from abnormal germ cells during fetal development or early life that later transform into cancer cells.
If I have a risk factor, what should I do?
If you have a known risk factor (for example, a history of undescended testicle, family history, or a genetic condition), tell your doctor. They may recommend more vigilant self-checks, periodic exams, or targeted imaging and blood tests in some cases. Discuss fertility concerns and sperm banking if treatment may affect sperm production.
How is Testicular Cancer Diagnosed and What Treatment Options Are Available?
Diagnosis typically begins with a physical exam, scrotal ultrasound, and blood tests for tumor marker levels. Treatment most often starts with radical inguinal orchiectomy (removal of the affected testicle) and may be followed by surveillance, chemotherapy, radiation, or additional surgery depending on the cancer type and stage.
If you or your doctor finds a lump or change in a testicle, the diagnostic pathway is rapid and focused. Early steps establish whether the abnormality is likely cancer and determine how far it may have spread so that an appropriate treatment plan can be made.
Diagnosis: tests and what they tell you
- Physical exam: Your doctor will feel both testicles to compare size, texture, and detect lumps or tenderness.
- Ultrasound of the scrotum: A painless imaging test that distinguishes a solid mass (more likely a tumor) from a fluid-filled cyst. Ultrasound is the primary imaging test for suspected testicular tumors.
- Blood tests — tumor marker levels: Blood levels of AFP (alpha‑fetoprotein), hCG (human chorionic gonadotropin), and LDH (lactate dehydrogenase) help indicate the presence and type of testicular cancer and are used for staging and follow-up.
- Imaging for staging: If cancer is likely, doctors may order CT scans (abdomen/chest) or chest X‑rays to check for lymph node involvement or distant spread (stage the disease).
If testing suggests cancer, the standard next step is an inguinal orchiectomy — surgical removal of the affected testicle through a groin incision. This both provides tissue for definitive diagnosis (pathology) and is usually the first therapeutic step.
Main treatment options
1. Surgery — Radical inguinal orchiectomy: Removal of the entire testicle and spermatic cord via a groin incision is the primary treatment. A testicular prosthesis can be offered later or at the time of surgery for cosmetic reasons. If imaging shows spread to retroperitoneal lymph nodes, a retroperitoneal lymph node dissection (RPLND) may be required.
2. Radiation therapy: Often used for seminomas (a type of testicular cancer) that have a higher sensitivity to radiation. Radiation targets nearby lymph nodes to reduce risk of recurrence in select stages.
3. Chemotherapy: Systemic chemotherapy (commonly regimens such as BEP — bleomycin, etoposide, cisplatin) treats cancer cells that may have spread beyond the testicle. Chemotherapy is the mainstay for advanced disease and for some cases with higher-risk features.
4. Active surveillance: For selected patients with very early-stage disease after orchiectomy, careful surveillance with regular physical exams, tumor marker blood tests, and periodic imaging is an accepted option to avoid overtreatment and the side effects of chemo or radiation.
How stage and type guide treatment
Treatment decisions depend on the histologic type (seminoma versus non‑seminoma), tumor marker levels, and stage (how far cancer has spread). Early-stage seminomas are often managed with surveillance or radiation; non‑seminomas may favor surveillance, RPLND, or chemotherapy depending on specific findings. Advanced stages typically require systemic chemotherapy.
Follow-up after treatment
Follow-up protocols include regular blood tests for tumor marker levels, periodic CT scans or chest X‑rays, and physical exams over several years to detect recurrence early. Your oncology team will outline a tailored schedule based on stage and treatment.
If you find a lump: Seek medical review promptly and, if available, bring any previous imaging or test results (ultrasounds, blood tests) to help your care team make quick, informed decisions.
Who is an Eligible Candidate for Testicular Cancer Treatment?
Any male diagnosed with testicular cancer should be considered for treatment. Which specific treatments are appropriate—surgery, chemotherapy, radiation, or surveillance—depends on the cancer type, stage, and the patient’s overall health and preferences.
In practice, virtually any man whose testicular cancer has been diagnosed is a candidate for care. The exact treatment pathway is individualized after doctors review the diagnosis, staging information, and the patient’s medical fitness and goals. Below are the main factors clinicians use to determine eligibility for specific treatments.
- Confirmed diagnosis: A definitive diagnosis (usually from pathology after an orchiectomy) is the first step that guides all further treatment decisions.
- Cancer type and stage: Is the tumor a seminoma or non‑seminoma? Has it spread to lymph nodes or beyond (Stage I, II, III)? These determine whether surveillance, radiation, chemotherapy, or additional surgery such as RPLND is recommended.
- Overall health and comorbidities: Ability to tolerate surgery or chemotherapy matters. Pre-existing heart, kidney, or lung conditions can influence drug choices (for example, cisplatin affects kidneys; bleomycin can affect lungs) and dosage decisions.
- Kidney and lung function: Before certain chemotherapy agents are used, tests check kidney and lung function to ensure treatment safety.
- Patient preferences and life plans: Patient priorities—fertility preservation, concern about side effects, desire to avoid immediate chemo or radiation—are integral to planning care.
Examples: a man with Stage I seminoma may be eligible for active surveillance after surgery, whereas a man with advanced non‑seminoma typically requires systemic chemotherapy and possibly additional surgery. Because many patients are young, fertility discussions (sperm banking before orchiectomy or chemotherapy) are a routine part of pre-treatment planning.
Questions to ask your doctor
- What is my exact diagnosis and stage?
- What are the pros and cons of surveillance versus immediate treatment for my case?
- Should I consider sperm banking now?
- Do I need any additional tests to confirm my eligibility for chemotherapy or surgery?
What Does Recovery from Testicular Cancer Treatment Involve?
Recovery after testicular cancer treatment varies by the therapy used. After orchiectomy most men can resume routine activities within weeks; recovery from chemotherapy can take months and often requires active symptom management. Long-term follow-up with blood tests and imaging is an essential part of ensuring a durable cure.
Recovery is both physical and emotional. Timelines differ depending on whether you had surgery, chemotherapy, radiation, or a combination. Below are practical expectations and tips for each phase to help you plan and know what to discuss with your care team.
Post‑Surgery (Orchiectomy) Recovery:
- Immediate (first few days): Most patients spend a short time in hospital (commonly 1–2 days) for pain control and early monitoring. Keep the incision clean and follow wound‑care instructions.
- First 2–4 weeks: Expect swelling and bruising of the scrotum that gradually subsides. Light activity is usually permitted within days; avoid heavy lifting or strenuous exercise until cleared by your surgeon.
- Long term: Many men choose a testicular prosthesis for cosmetic reasons (either at initial surgery or later). Removal of one testicle generally does not significantly affect testosterone or fertility because the remaining testicle often compensates; discuss hormone checks if symptoms of low testosterone appear.
Post‑Chemotherapy Recovery:
- During treatment: Chemotherapy commonly causes fatigue, nausea, hair loss, mouth sores, and a temporarily weakened immune system. Your oncology team will offer supportive medications (antiemetics, growth factors) and guidance to manage side effects.
- After finishing chemo: Recovery can take weeks to months. Blood counts and organ function (kidney, liver) are monitored until they return to safe levels. Hair usually regrows and many acute side effects resolve over time.
- Possible long‑term effects: Some patients experience lasting neuropathy (numbness or tingling), hearing changes, or kidney issues depending on drugs used (for example, cisplatin-related risks). Discuss baseline and follow‑up testing with your oncologist.
Post‑Radiation Recovery:
- During and shortly after treatment: Fatigue and localized skin irritation are common; these typically improve within weeks.
- Long term: Radiation can temporarily reduce sperm counts and carries a small long‑term risk of secondary cancers in the treated field; sperm banking is often recommended if future fertility is a concern.
Emotional and practical recovery: Beyond physical healing, many people face anxiety about recurrence, body image concerns, or fertility worries. Support groups, counseling, and open conversations with your medical team and family are important. Practical tips include scheduling rest periods, gradual return to activity, and nutrition to support healing.
Follow‑up and surveillance: Ongoing monitoring after treatment typically includes regular physical exams, blood tests for tumor marker levels, and periodic imaging (CT or chest X‑ray) for several years. Adhering to your follow‑up schedule is key to catching any recurrence early when treatment is most effective.
Practical tips and fertility planning
- If chemotherapy is likely, consider sperm banking before treatment — discuss timing with your doctor.
- Ask your team about protective measures (hydration protocols for kidneys, lung monitoring if bleomycin is used).
- Keep a recovery diary (symptoms, medications, appointments) and bring it to follow‑up visits.
What are the Potential Risks and Side Effects of Testicular Cancer Treatment?
Treatments for testicular cancer—surgery, chemotherapy, and radiation—are effective but carry potential short‑ and long‑term risks. Common immediate issues include surgical complications (infection, bleeding) and treatment side effects (fatigue, nausea, hair loss); long‑term concerns can include fertility changes and rare secondary cancers.
Understanding possible risks helps you weigh benefits and prepare. Below is a practical overview of the typical side effects and longer‑term risks to discuss with your care team.
Risks and side effects of orchiectomy (surgery)
- Immediate: pain, bleeding, wound infection, swelling and bruising of the scrotum.
- Long‑term: most men maintain normal testosterone and fertility because the remaining testicle generally compensates, but a minority may experience low testosterone symptoms (fatigue, low libido) and could need hormone replacement.
Risks and side effects of chemotherapy
Chemotherapy targets cancer cells systemically but can affect healthy cells too. Your oncology team will explain which regimen is planned and how side effects will be managed.
- Common, usually temporary: nausea, vomiting, fatigue, hair loss, mouth sores, appetite changes, and low blood counts (myelosuppression) that raise infection risk.
- Serious or long‑term: peripheral neuropathy (numbness/tingling), hearing changes (ototoxicity), kidney function impact (cisplatin), and potential lung toxicity with bleomycin (requires monitoring). There is also a small increased lifetime risk of secondary cancers after certain regimens.
- Fertility: Chemotherapy can reduce sperm production temporarily or, less commonly, permanently. Sperm banking before treatment is strongly recommended for men who may want children in the future.
Risks and side effects of radiation therapy
- Short term: fatigue, localized skin irritation, and sometimes gastrointestinal upset depending on the field treated.
- Long term: temporary or longer‑term reduction in sperm count (often recovers), and a small increased risk of secondary cancers in the radiation field many years later.
How doctors manage and reduce risks
Oncology teams use pre‑treatment testing (blood levels, kidney and lung function tests, hearing checks) and protective measures to lower complication risk. Examples include hydration protocols to protect kidneys during cisplatin, pulmonary monitoring when bleomycin is used, and supportive medications to prevent nausea and infections.
Questions to ask about side effects
- How likely are specific long‑term effects with the treatment you recommend?
- What monitoring will you do for kidney, lung, and hearing function?
- Should I bank sperm before treatment, and how soon can I expect fertility to recover?
Your care team will balance risks against the goal of curing cancer. Advances in supportive care have greatly improved the safety and tolerability of testicular cancer treatment, but open discussion about both short‑ and long‑term effects is essential to informed decisions.
How Much Does Testicular Cancer Treatment Cost Worldwide?
Testicular cancer treatment costs vary widely by country, facility, and the care pathway required. In higher‑cost systems (for example, the US), an orchiectomy alone can run into the tens of thousands, while complex chemotherapy courses and inpatient care can push total costs much higher. Many countries such as India, Turkey, Mexico, and Thailand offer comparable-quality care at substantially lower prices for many procedures.
Cost is an important consideration for people facing testicular cancer, especially where insurance coverage is limited or deductibles are high. Total expense depends on the stage at diagnosis, whether chemotherapy or radiation is required, the number of chemotherapy cycles, hospital stay duration, and whether additional surgeries (like RPLND) are needed. The table below provides rough estimates to help you compare options; these are illustrative ranges and should be confirmed with providers.
Cost Comparison for Testicular Cancer Treatment (Estimates in USD)
| CountryRadical Inguinal Orchiectomy (Surgery Only)Chemotherapy Cycle (per cycle, typically 3–4 cycles)Full Treatment Course (Surgery + Chemo/Radiation)* | |||
| United States | $15,000 – $35,000 | $10,000 – $30,000+ | $50,000 – $150,000+ |
| United Kingdom (Private) | $8,000 – $20,000 | $5,000 – $15,000 | $30,000 – $80,000 |
| Germany | $10,000 – $25,000 | $6,000 – $20,000 | $35,000 – $90,000 |
| Turkey | $3,000 – $8,000 | $2,000 – $5,000 | $10,000 – $30,000 |
| India | $2,500 – $7,000 | $1,500 – $4,000 | $8,000 – $25,000 |
| Mexico | $4,000 – $10,000 | $2,500 – $6,000 | $12,000 – $35,000 |
| Thailand | $3,500 – $9,000 | $2,000 – $5,500 | $10,000 – $32,000 |
*Note: “Full Treatment Course” costs are highly variable and depend on cancer stage, the number of chemotherapy cycles, need for radiation, hospital stay length, and complications. These are broad estimates and do not include travel, accommodation, or ancillary costs. Always request a personalized quote.
What these estimates do and do not include: ranges may cover surgeon and hospital fees, anesthesia, basic inpatient care, and standard chemotherapy drugs, but they may exclude high-cost branded drugs, ICU stays, prosthetic testicle, extended rehab, or follow‑up imaging. Insurance coverage, negotiated hospital rates, and government subsidies can dramatically change your out‑of‑pocket cost.
How to get a personalized cost estimate
- Gather your records: pathology reports, imaging (DICOM if possible), tumor marker levels, and current medications.
- Ask for an itemized quote that lists what’s included (surgeon fees, drugs, hospital stay, follow‑up visits) and what’s not (travel, accommodation, complications).
- Check whether the provider offers bundled packages and what post‑discharge follow‑up is included.
- Verify refund and complication policies, and whether your home insurance will reimburse part of the cost.
Because costs change and vary by individual case, treat the table above as a starting point and confirm current pricing with hospitals or medical facilitators. If you’d like, the next sections explain why many patients consider treatment abroad and how to evaluate safe, high‑quality providers.
Why Should I Consider Testicular Cancer Treatment Abroad?
Seeking testicular cancer treatment abroad can offer substantial cost savings, faster access to care, and access to high-quality, accredited facilities and experienced specialists. For many people, these advantages make medical tourism a viable option when local care is expensive or delayed.
For patients facing high out‑of‑pocket costs, long wait times, or limited local expertise, traveling to another country for treatment may provide timely, affordable access to oncologic care. Below are common benefits — and a few important tradeoffs to consider — when evaluating treatment abroad.
- Cost savings: Many international centers offer procedures and chemotherapy regimens at significantly lower prices than Western hospitals, often helping patients reduce total treatment costs by a large margin.
- Faster access to care: Some patients can get quicker appointments, diagnostics, and surgery overseas than in systems with long waiting lists — an important advantage when time matters.
- World‑class facilities and expertise: Many hospitals abroad are accredited by recognized bodies (for example, JCI) and employ oncologists and surgeons trained internationally, with experience treating testicular cancer and using advanced technology.
- Convenience packages: Some providers offer bundled services that include treatment planning, accommodation, airport transfers, and interpreter support, simplifying logistics for patients and families.
- Privacy and personalized care: Traveling for treatment can offer greater privacy and sometimes more individualized attention from care coordinators.
Tradeoffs and when not to travel
Traveling for care also has downsides: continuity of follow‑up can be harder, complications may require local care after you return home, and travel itself can be stressful or risky if you’re medically unstable. Consider staying local if you need urgent emergency care, are medically fragile, or if coordination between international and local teams would be difficult.
If you’re considering treatment abroad, the next sections explain which countries often offer the best value and how to evaluate providers to ensure safety and quality.
Which Countries Offer the Best Value for Testicular Cancer Treatment?
Top countries for value in testicular cancer treatment often include India, Turkey, Mexico, Thailand, and South Korea. These destinations frequently combine experienced specialists and modern facilities with lower pricing for many procedures, making them popular choices for patients seeking high-quality, cost-effective care.
When considering treatment testicular cancer abroad, several factors matter beyond price: facility accreditation, surgeon and oncology experience, availability of multidisciplinary care (urology, medical oncology, radiation oncology), and reliable post‑treatment follow‑up. The countries below are frequently chosen because they offer strong combinations of these features.
- India: Known for many JCI‑accredited hospitals and oncology centers, India offers experienced surgeons and oncologists often trained internationally, with highly competitive pricing for surgeries, chemotherapy, and supportive care.
- Turkey: A growing medical tourism hub, Turkey has modern hospitals, internationally trained teams, and geographic convenience for patients from Europe, the Middle East, and Asia. Many centers offer comprehensive cancer packages.
- Mexico: Attractive for North American patients because of proximity and shorter travel times. Several Mexican hospitals provide JCI‑accredited oncology services and competitive pricing.
- Thailand: Thai hospitals—particularly in Bangkok—are noted for patient service, strong oncology programs, and bundled medical tourism support that includes accommodation and interpreter services.
- South Korea: While sometimes pricier than other options, South Korea is recognized for medical innovation and high technical standards in oncology care and may be a choice for patients seeking cutting‑edge diagnostics and treatment.
Practical considerations: check whether individual hospitals in your chosen country are accredited (for example, JCI), verify the treating team’s experience with testicular cancers, confirm language support, ask about typical wait times, and request references or patient outcomes when possible. Remember that not every hospital in these countries will offer the same level of care—do your due diligence for the particular clinic and team you plan to use.
What Should I Expect When Traveling Abroad for Testicular Cancer Treatment?
When traveling abroad for testicular cancer care, you’ll manage logistics such as visas, flights, and accommodation while coordinating with the treating hospital. Many international centers offer patient coordinators, interpreters, and all‑inclusive packages to streamline the process from initial consultation through follow‑up.
Planning ahead reduces stress and helps ensure your medical trip goes smoothly. Below is a practical walkthrough of the typical steps, plus a checklist of the documents and timelines you’ll likely need.
Initial consultation and preparation
- Send medical records: Provide pathology reports, imaging (ideally DICOM files for CT/MRI), ultrasound reports, and recent tumor marker blood tests (AFP, hCG, LDH). The treating team will give an initial assessment, recommended tests, and a cost estimate.
- Get a pre‑trip plan: Confirm the proposed timeline for arrival, pre‑treatment testing, the procedure or chemo schedule, expected hospital stay, and recommended recovery time before travel home.
Travel logistics checklist
- Visa and entry: Verify visa requirements (medical visas are available in many countries); allow several weeks for processing.
- Flights and transport: Book direct flights where possible to minimize travel stress. Arrange airport transfer with the hospital or facilitator.
- Accommodation: Choose lodging recommended by the hospital (some offer patient guesthouses) and confirm proximity to the clinic.
- Travel companion: Bring a friend or family member if possible — they help with logistics and recovery support.
Documents to bring (digital and paper copies)
- Pathology and biopsy reports
- Imaging files (CT, ultrasound — DICOM preferred) and reports
- Recent blood tests, including tumor marker levels (AFP, hCG, LDH)
- List of current medications and allergies
- Passport, insurance details, and emergency contact information
What happens on arrival and during pre‑treatment
- Airport pickup and orientation: Many hospitals arrange transfers and an initial meeting with a patient coordinator.
- Repeat or confirm tests: The hospital may repeat imaging or blood tests to confirm staging and treatment plans.
- Consent and scheduling: Expect discussions about risks/benefits and signing consent forms before procedures.
Treatment, recovery, follow‑up, and departure
- Treatment and in‑hospital care: Hospitals manage post‑operative care and chemotherapy side effects; expect clear instructions about medications and activity limitations.
- Follow‑up plan: Before you leave, obtain a complete medical report, prescriptions, and a clear follow‑up schedule (dates for tumor marker tests and imaging) to share with your local doctor.
- Emergencies and complications: Ask the hospital how to access urgent care if problems arise after you return home and whether they offer remote follow‑up or telemedicine.
Timing — sample planning timeline
Start planning at least 4–8 weeks before planned surgery when possible. Typical steps: initial remote consult and records review (week −6), visa and travel booking (week −5 to −3), arrival and pre‑op tests (day −3 to −1), procedure (day 0), inpatient recovery (1–5 days depending on procedure), short stay post‑discharge as advised (1–4 weeks), then return home with remote or in‑person follow‑up arranged.
Medical tourism facilitators can help coordinate these steps, but confirm credentials and read reviews. If you’re medically unstable, needing urgent emergency care, or traveling poses significant risk, prioritize local treatment and seek advice from your doctor.
How Can I Ensure Safety and Quality of Testicular Cancer Treatment Abroad?
To reduce risk when seeking testicular cancer treatment abroad, choose internationally accredited hospitals, verify the treating doctors’ credentials and experience, read independent patient reviews, request a detailed treatment plan and itemized quote, and get a second opinion at home when possible.
Quality and safety vary between providers, so due diligence is essential. Below is a practical checklist and red‑flag guide to help you evaluate international hospitals, doctors, and facilitators before committing to travel for care.
Checklist: what to verify
- Facility accreditation: Look for recognized accreditations such as Joint Commission International (JCI) or other national/international oncology credentials.
- Doctor credentials: Verify the surgeon’s and oncologist’s board certifications, years of experience treating testicular cancers, and case volume. Check training and any international fellowships.
- Clinical outcomes and transparency: Ask for published outcome data or survival/cure rates for similar cases, complication and readmission rates, and average length of stay.
- Patient reviews and references: Read independent reviews and request patient references or case studies—ideally with clinical follow‑up details.
- Detailed written plan and itemized quote: Obtain a clear treatment plan listing procedures, chemotherapy regimens, expected hospital days, follow‑up tests, and a transparent cost breakdown.
- Communication and language support: Ensure you have reliable translation services and direct lines to care coordinators for questions before, during, and after treatment.
- Medical records in transferable format: Request copies of all reports and imaging in shareable formats (DICOM for scans) so local and international teams can coordinate care.
Red flags to avoid
- Vague or verbal cost estimates without itemization, or pressure to pay large sums upfront without a contract.
- Hospitals unwilling to share surgeon credentials, outcomes data, or references.
- No clear plan for post‑treatment follow‑up or refusal to provide full medical records.
- Exaggerated promises (e.g., guaranteed cure) or reluctance to discuss risks and complications.
Questions to ask the hospital or doctor
- How many testicular cancer cases like mine has your team treated in the past year?
- Can you share complication rates, readmission rates, and typical recovery times for this procedure?
- Will you provide a complete written plan, expected timeline, and itemized costs?
- How will you coordinate follow‑up care with my local doctor after I return home?
Consider getting a second opinion from a local oncologist before traveling. If you use a medical tourism facilitator, verify their reputation, read independent reviews, and ensure they do not replace clinical decision‑making by certified physicians. Careful preparation and transparent communication significantly lower risk and improve the likelihood of a successful, well‑coordinated testicular cancer treatment abroad.
What are Patient Success Stories and Outcomes for Testicular Cancer Treatment Abroad?
Many patients who seek testicular cancer treatment abroad report excellent clinical outcomes, meaningful cost savings, and positive overall experiences with coordinated care — especially when treated early. While individual stories are encouraging, outcomes vary by stage, treatment type, and the specific facility chosen.
Testicular cancer generally has high cure rates compared with many other cancers, particularly when diagnosed at an early stage. International centers that follow established oncologic protocols can deliver outcomes comparable to those in Western countries, provided you select an accredited hospital and an experienced multidisciplinary team.
Common themes in patient-reported successes:
- High cure and survival rates: For localized testicular cancer, five‑year survival commonly exceeds 95% in many settings when standard treatments are applied; advanced cases also have substantially improved outcomes with modern chemotherapy.
- Significant cost savings: Patients often report saving large sums by choosing treatment abroad, freeing resources for recovery, travel, or family support.
- Access to experienced teams and technology: Many success stories highlight prompt access to multidisciplinary care (urology, medical oncology, radiation oncology) and advanced diagnostics or chemotherapy protocols.
- Personalized and supportive care: International patient departments often provide care coordination, interpreters, and accommodation assistance that patients find reassuring during treatment.
Example (anonymized, illustrative): A patient from the U.S. received orchiectomy and adjuvant chemotherapy in Turkey with coordinated follow‑up; he reported a smooth recovery, lower total cost than local care, and timely return to work. Another patient from Canada described faster access to diagnosis and treatment in India, reducing anxiety during the diagnostic window.
A balanced view: while many patient stories are positive, not every experience is the same. Some patients face logistical challenges, communication gaps, or unexpected complications. When evaluating testimonials, look for clinical details (stage, treatments given, follow‑up duration) and verify outcomes where possible.
If you’re considering treatment abroad, request outcome data from the clinic (survival rates, complication rates) and ask for references to speak with former patients. Combining these steps with the safety checklist in the previous section will help you choose a high‑quality option that maximizes the chance of a successful outcome.
Take the Next Step with DGS Healthcare
Ready to explore safe, vetted testicular cancer treatment options abroad? DGS Healthcare can help you discover accredited clinics, compare treatment testicular cancer plans and prices, and get a personalized, itemized quote.
DGS Healthcare reviews facilities and provides support with logistics and communication — request a quote and expect a response within a few business days.
Before sharing medical records, review privacy policies and confirm how your data will be used. For urgent medical advice, contact a local doctor first.
