Thyroid Cancer Treatment
Overview: Thyroid cancer is a generally treatable form of cancer that starts in the thyroid gland. Treatment most often includes surgery and, for certain types (especially differentiated cancers), may be followed by radioactive iodine therapy; many patients also consider international care for cost savings and access to specialized expertise.
Navigating Thyroid Cancer: Your Guide to Treatment & Global Care Options
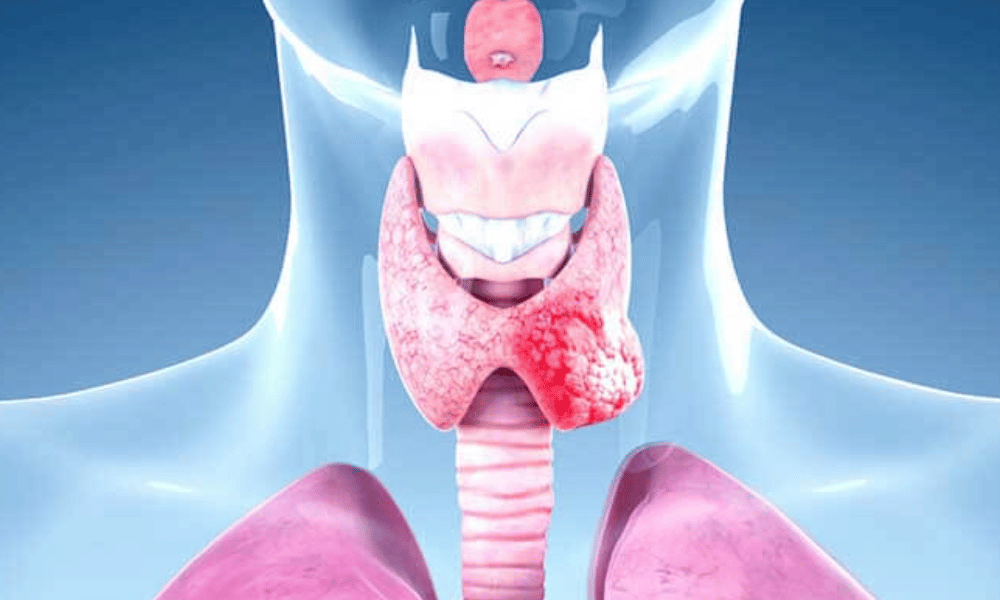
A diagnosis of thyroid cancer can raise many immediate questions: What type of thyroid cancer do I have? What treatment choices are best for me? The thyroid is a small, butterfly-shaped gland at the base of the neck that makes hormones essential for metabolism. Fortunately, many types of thyroid cancer are highly treatable, particularly when found early.
This guide explains the most common symptoms and causes, walks through diagnostic tests and treatment options (from surgery to hormone therapy and targeted drugs), and outlines what to expect during recovery. It also covers practical considerations for people exploring care abroad—why patients choose international centers, how to compare clinics, and what logistics to plan.
If you’re searching for “affordable thyroid surgery,” “best countries for thyroid cancer treatment,” or “what to expect after thyroidectomy,” read on. We’ll provide clear, patient-focused information to help you understand options, prepare for consultations, and take the next steps with confidence.
What are the Common Symptoms of Thyroid Cancer?
The most common symptom of thyroid cancer is a lump or nodule in the neck, which is often painless. Other possible signs include changes to your voice, trouble swallowing, neck pain, or swollen lymph nodes.
Thyroid cancer frequently has no symptoms in its earliest stages and is often found incidentally during imaging for another reason. As the tumor grows, these symptoms may appear — recognizing them and acting promptly can help with early diagnosis.
- A lump or nodule in the neck: Usually felt just below the Adam’s apple. Thyroid nodules often move slightly when you swallow. Many nodules are benign, but any new or growing thyroid nodule should be evaluated by a doctor.
- Hoarseness or other voice changes: Persistent hoarseness not caused by a cold may occur if a tumor irritates or presses on the nerves that control the vocal cords.
- Difficulty swallowing (dysphagia): A larger thyroid growth can press on the esophagus and create a sensation that food is getting stuck.
- Trouble breathing: Rare but possible if a tumor becomes large enough to compress the windpipe, causing shortness of breath or a tight feeling in the neck.
- Pain in the neck and throat: While many thyroid cancers are painless, some people experience localized pain that can radiate to the ears.
- Swollen lymph nodes in the neck: Enlarged nodes on one side of the neck can indicate the cancer has spread to nearby lymph nodes (nodes).
If you notice any persistent symptom — especially a new lump in your neck — see a healthcare professional. Typical diagnostic steps include a physical exam, thyroid ultrasound, and, if indicated, a fine-needle aspiration biopsy (a common test to check whether a thyroid nodule is cancerous).
Example: A person undergoing a routine carotid ultrasound for vascular screening may have a thyroid nodule discovered incidentally; that nodule would then be evaluated for size, appearance on imaging, and possibly sampled with a biopsy.
If you have a persistent lump or other concerning symptom, don’t delay — get evaluated by your primary care doctor, an ENT specialist, or an endocrinologist to arrange appropriate tests and next steps.
What Causes Thyroid Cancer and Who is at Risk?
The exact cause of most thyroid cancers is unknown, but several risk factors are associated with a higher likelihood of developing the disease — including prior radiation exposure, certain inherited syndromes, family history, and biological factors like sex and age.
While many cases arise without an identifiable cause, understanding recognized risks can help people and their clinicians decide when to monitor more closely or pursue further testing. Key risk factors include:
- Radiation exposure: The strongest known environmental risk — especially radiation to the head and neck during childhood (for example, past therapeutic radiation or fallout exposure).
- Family history and inherited syndromes: A close relative with thyroid cancer raises risk, particularly for medullary thyroid cancer. Certain inherited conditions — such as Multiple Endocrine Neoplasia type 2 (MEN2), Familial Adenomatous Polyposis (FAP), and Cowden syndrome — are linked to higher rates of specific thyroid cancer types. MEN2, for example, is an inherited disorder that often leads to medullary thyroid tumors and may prompt genetic testing for family members.
- Gender and age: Thyroid cancer is diagnosed more often in women than men (several studies report roughly a 2–3× higher incidence in women). Differentiated thyroid cancers (papillary and follicular types) commonly present between ages 20–55, while more aggressive forms like anaplastic thyroid cancer are more frequent in older adults.
- Iodine intake: Diets very low in iodine have been associated with higher rates of follicular thyroid cancer in some populations; conversely, very high iodine intake has been linked in some studies to papillary thyroid changes. These relationships vary by region and overall diet.
- Metabolic factors: Emerging research suggests possible links between obesity, diabetes, and a modestly increased thyroid cancer risk, but more studies are needed to confirm causation.
Who should be more vigilant? People with a history of head or neck radiation, a family history of thyroid cancer (especially medullary), or known genetic syndromes like MEN2 should discuss tailored surveillance with their doctor. Genetic counseling and testing are often recommended when inherited syndromes are suspected.
If you have risk factors, bring them up with your primary care provider or an endocrinologist. They can recommend appropriate monitoring (clinical exams, ultrasound) and advise whether genetic testing or earlier referral is warranted.
What Types of Thyroid Cancer Treatments Are Available?
The primary treatment for most thyroid cancers is surgery (thyroidectomy). Depending on the cancer type and stage, surgery may be followed by radioactive iodine (RAI), lifelong thyroid hormone replacement, external beam radiation, chemotherapy, or targeted drug therapy.
Treatment is individualized based on the type of thyroid cancer (papillary, follicular, medullary, anaplastic), the stage, and your overall health. Below are the main options, with brief guidance on when they are used and what to expect.
- Surgery (Thyroidectomy): The cornerstone of treatment for most thyroid cancers.
- Total thyroidectomy — removal of the entire thyroid gland. Common for larger tumors, multifocal disease, or when RAI is likely to be used afterward. Expect a hospital stay of 1–3 days for uncomplicated cases.
- Lobectomy (hemithyroidectomy) — removal of one lobe. May be appropriate for small, low-risk papillary or follicular tumors; patients may not require lifelong thyroid hormone if enough gland remains.
- Lymph node dissection — removal of involved lymph nodes when cancer has spread to nearby nodes.
- Radioactive iodine (RAI) therapy: Used primarily after surgery for differentiated thyroid cancers (papillary and follicular) to destroy remaining thyroid tissue or microscopic cancer cells. Because thyroid cells absorb iodine, RAI selectively targets those cells. Not typically effective for medullary or anaplastic types. Discuss with your team whether your tumor’s type, size, and risk factors indicate RAI; dosing and isolation recommendations vary by protocol.
- Thyroid hormone therapy (levothyroxine): After total thyroidectomy most patients take synthetic thyroid hormone daily for life to replace the gland’s function and to suppress TSH when appropriate (TSH suppression reduces the chance of stimulating remaining cancer cells). Regular blood tests guide dosing.
- External beam radiation therapy: Reserved for more aggressive or locally advanced tumors (for example, anaplastic thyroid cancer) or when surgery/RAI are not options. It can help control local disease but carries typical radiation side effects.
- Chemotherapy: Rarely used for differentiated thyroid cancers; may be considered for anaplastic thyroid cancer or widely metastatic disease not responsive to other therapies.
- Targeted drug therapy: For advanced cancers that no longer respond to standard treatments, targeted agents (for example, tyrosine kinase inhibitors or TKIs) act on specific molecular pathways in cancer cells. Molecular testing of tumor cells can identify actionable mutations and guide targeted therapy choices.
- Observation (active surveillance): An option for very small, low-risk papillary microcarcinomas. Instead of immediate surgery, the nodule is monitored with periodic ultrasound and clinical exams; treatment is offered if growth or concerning changes occur.
How treatment is chosen: tumor type (papillary, follicular, medullary, anaplastic), size, lymph node involvement, patient age, and personal preferences all influence decisions. For example, papillary thyroid cancer often responds well to surgery ± RAI; medullary thyroid cancer may prompt genetic testing and a surgical approach focused on the gland and affected nodes; anaplastic cancer typically requires aggressive multimodality therapy.
Questions to ask your team: Which surgery do you recommend and why? Will I need RAI? What tests will you run on the tumor (molecular profiling)? How long is the expected hospital stay and follow-up schedule? Getting clear answers helps you plan recovery and any travel if seeking care abroad.
Who is Eligible for Thyroid Cancer Treatment Abroad?
Most patients diagnosed with thyroid cancer can explore treatment abroad, provided they have a confirmed diagnosis and are medically stable to travel. Suitability for specific treatments depends on the tumor type, stage, and the patient’s overall health.
Eligibility for international care generally mirrors eligibility for local care, but with added travel considerations. The following factors determine feasibility and help international clinics assess cases:
- Definitive diagnosis and medical records: You should have biopsy results, imaging (ultrasound/CT/MRI), pathology reports, and blood tests. International teams require complete records to recommend an appropriate plan.
- Medical stability for travel: Patients must be well enough to fly. Those with advanced disease or significant comorbidities may need special arrangements (medical escorts, ground transport) or stabilization at home before travel.
- Cancer type and stage: Most differentiated cancers (papillary, follicular) are routinely treated abroad. Medullary cases may prompt genetic counseling first. Aggressive anaplastic cancers or patients needing urgent, complex care may be less suitable for immediate travel, though specialist centers sometimes offer advanced therapies.
- Overall health and comorbidities: Well-controlled chronic conditions usually do not preclude travel, but severe heart, lung, or other systemic issues may. A pre-travel medical clearance is advised.
- Practical readiness: Financial ability to cover treatment, travel, accommodation, and follow-up, plus valid passport/visa, are required. Many patients arrange a companion to assist during recovery.
Checklist before you commit to treatment abroad:
- Gather and send complete medical records (scans, biopsy, labs) for review.
- Obtain a pre-travel medical clearance from your physician stating you are fit to fly.
- Request an itemized quote that lists surgeon fees, hospital stay, anesthesia, pathology, and any expected RAI or follow-up tests.
- Confirm visa/passport requirements and plan for a companion to assist during recovery.
Before committing, arrange a remote consultation with the international team or facilitator (many services like PlacidWay provide this). They will review records, confirm suitability, and outline logistics and estimated timelines.
How Long is Recovery After Thyroid Cancer Surgery?
Full recovery after thyroid cancer surgery typically takes 2–4 weeks for most people, with a hospital stay of 1–3 days for uncomplicated cases. More extensive surgery or additional treatments (like RAI) can lengthen recovery time.
Recovery varies by procedure, individual healing, and whether lymph nodes were removed or RAI is planned. Below is a general timeline to help you plan, including timeframes relevant for patients traveling for care.
- Immediate post-op (hospital stay: 1–3 days): You’ll wake with a dressing on the neck. Expect mild pain, sore throat, and possibly hoarseness. Medical teams monitor for bleeding and low calcium (hypocalcemia) if parathyroid glands were affected.
- First week home: Incision care and rest are important. Avoid heavy lifting and strenuous activity. Light walking is encouraged. Voice changes and neck stiffness are common and often improve over days to weeks.
- Weeks 2–4: Many people return to light work after 1–2 weeks; full return and strenuous activity usually take 3–4 weeks or longer depending on job demands and healing.
- Long-term (months to years): If you had a total thyroidectomy you will start levothyroxine (thyroid hormone) replacement and require regular blood tests to fine-tune dosing. If RAI is planned, additional isolation and follow-up testing will be required.
Sample international patient timeline: remote consultation and records review (2–4 weeks), travel for surgery and 1–3 day hospital stay, local recovery and follow-up checks for 1–3 weeks, then return home with coordinated follow-up plan. Ask your international team for a written timeline and a travel-safe medical clearance before booking flights.
Tip: Before travel, confirm how post-operative care and blood tests (TSH, calcium) will be coordinated between the treating center abroad and your local doctor to ensure seamless follow-up.
What Are the Risks and Side Effects of Thyroid Cancer Treatment?
Treatments for thyroid cancer — especially surgery and radioactive iodine — are generally safe but can have side effects such as voice changes, low calcium (from parathyroid disturbance), bleeding, infection, and temporary symptoms after RAI like dry mouth or fatigue.
All medical treatments carry potential risks. Discussing these with your surgeon and oncology team helps you understand which are most relevant to your case and how they will be prevented or managed.
Risks of Thyroidectomy (Surgery):
- Voice changes: Temporary hoarseness or altered voice is common; permanent voice loss is uncommon. Surgeons use intraoperative nerve monitoring and careful technique to reduce risk. If voice changes persist, referral to an ENT or speech therapist is available.
- Hypoparathyroidism (low calcium): If parathyroid glands are damaged or removed, patients can develop low calcium requiring supplements. Many centers try to preserve parathyroids or autotransplant them; calcium levels are checked after surgery and supplements started if needed.
- Bleeding and hematoma: Rare but potentially serious; early post-op monitoring reduces risk and allows prompt treatment if bleeding occurs.
- Infection and scarring: Surgical-site infection is uncommon; a visible neck scar is typical but often placed in a skin crease and can fade over time.
Side Effects of Radioactive Iodine (RAI) Therapy:
- Salivary gland effects: Dry mouth, altered taste, or salivary swelling can occur; staying hydrated and using saliva stimulants (sour candies) may help.
- Neck discomfort, nausea, fatigue: Usually short-lived; follow-up care includes symptom management and monitoring.
- Fertility and long-term risks: High doses of RAI can temporarily affect fertility — discuss family planning with your team before treatment. There is a very small, long-term theoretical risk of second cancers; for aggressive disease the benefits of RAI usually outweigh this minimal risk.
Side Effects of Thyroid Hormone Therapy:
- Levothyroxine dosing is individualized; over- or under-dosing produces symptoms of hyper- or hypothyroidism respectively. Regular blood tests (TSH, free T4) guide safe dosing adjustments.
Side Effects of External Beam Radiation, Chemotherapy, and Targeted Therapies:
- These vary by treatment and dose. Possible effects include fatigue, skin changes, nausea, hair loss, and drug-specific toxicities for targeted agents; monitoring and supportive care minimize impact.
How risks are managed: Experienced surgical teams use measures such as intraoperative nerve monitoring and parathyroid preservation to reduce complications. Your medical team will outline monitoring plans (blood tests for calcium and thyroid function, voice checks) and provide management strategies like calcium supplementation or referrals to specialists (ENT, speech therapy, fertility specialists) when needed.
Questions to ask your team: What are my specific complication rates? How will you monitor calcium and thyroid hormone levels after surgery? Should I see a fertility counselor before RAI? Getting written answers helps you compare options and prepare for recovery.
Worldwide Cost Comparison for Thyroid Cancer Treatment
The cost of thyroid cancer treatment, especially surgery, varies significantly by country and by the complexity of the case. In Western countries prices can be substantially higher, while medical tourism destinations often provide comparable care at a lower price — though figures are estimates and will depend on the specifics of your treatment plan.
Many people consider treatment abroad primarily because of cost differences. Exact pricing depends on the procedure (total thyroidectomy vs lobectomy), whether lymph node dissection is required, and inclusion of additional services such as radioactive iodine (RAI) therapy, pathology, and follow-up care. The table below gives approximate ranges to help you compare countries and start conversations with clinics.
| Country/RegionEstimated Cost Range (USD) for Total Thyroidectomy*Typical Inclusions | ||
| USA/Canada | $25,000 – $60,000+ | Surgeon’s fee, anesthesia, hospital stay, pathology; RAI and follow-up often billed separately. |
| Western Europe (e.g., UK, Germany) | $20,000 – $50,000+ | Surgeon’s fee, anesthesia, hospital stay, pathology; RAI may be additional. |
| Turkey | $8,000 – $18,000 | Surgery, hospital stay, consultations, and post-op care; packages often available. |
| Mexico | $7,000 – $15,000 | Surgery, hospital stay, consultations; proximity benefits for North American patients. |
| India | $5,000 – $12,000 | Surgery, hospital stay, pre/post-op care; many hospitals offer international patient packages. |
| South Korea | $10,000 – $25,000 | Advanced surgical techniques and state-of-the-art facilities; molecular testing commonly available. |
| Thailand | $6,000 – $14,000 | Surgery, hospital stay, and often accommodation packages for international patients. |
*Estimates only: costs vary by clinic, surgeon experience, case complexity, and whether additional therapies (e.g., radioactive iodine, lymph node dissection, molecular tests) are required. Always request an itemized quote.
Cost checklist — what to ask clinics when comparing quotes:
- Is the surgeon’s fee, anesthesia, and hospital stay included? Are pathology and imaging included?
- Does the quote include lymph node dissection if needed, RAI therapy, or molecular testing?
- What is the expected length of stay and which post-op visits or blood tests (TSH, calcium) are covered?
- Are travel assistance, accommodation, and interpreter services included in any package?
Sample difference: a lobectomy (one lobe removed) will generally cost less than a total thyroidectomy plus RAI and lymph node dissection; ask clinics to provide separate pricing for these scenarios so you can compare like-for-like.
Practical tips: request at least two detailed quotes, verify hospital accreditation (e.g., JCI where applicable), check surgeon experience with thyroid surgeries, and confirm how follow-up care and testing will be coordinated once you return home.
Take the Next Step with DGS Healthcare
Ready to explore thyroid cancer treatment options abroad? Get a free, personalized quote and clinic comparison to find care that fits your needs, budget, and timeline.
Trusted support: international patient coordinators, JCI-partnered hospitals (where available), and help coordinating records, visas, and follow-up. Have your recent medical records ready (diagnosis, imaging, biopsy/pathology, and blood tests) to speed up the review and quote process.
