Uterine Cancer Treatment
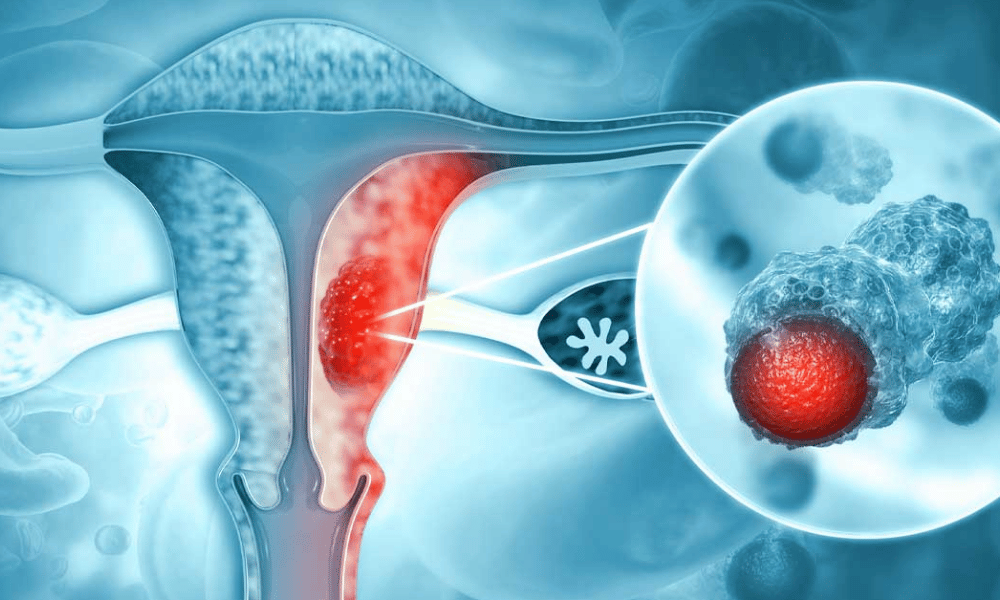
Uterine cancer — most commonly endometrial cancer — is abnormal growth of cells in the lining of the uterus (endometrium). Treatments include surgery (hysterectomy), radiation, chemotherapy, hormone therapy, and targeted therapy, chosen based on cancer type and stage. It most often affects women after menopause; incidence rises with age. (Source: American Cancer Society)
Navigating Uterine Cancer: Comprehensive Treatment & Medical Tourism Options
A diagnosis of uterine cancer — most often endometrial cancer — raises urgent questions about symptoms, diagnosis, and treatment. This guide explains what uterine and endometrial cancers are, who is at risk, and how common treatments (surgery, radiation, chemotherapy, hormone or targeted therapy) work, so you can make informed decisions about your care.
Many patients also consider treatment abroad to access advanced technology (for example, robotic surgery), shorter wait times, or lower costs. Medical tourism can offer real benefits for some people, but it also carries practical and continuity-of-care considerations — we outline both so you can weigh options carefully. (Source: American Cancer Society)
What you’ll learn in this article: a) common symptoms and when to seek urgent care, b) risk factors and prevention steps, c) standard and emerging uterine cancer treatments by stage, d) what to expect if you travel for care, and e) how to choose a safe, accredited facility abroad.
What are the common symptoms of uterine cancer?
The most common symptom of uterine cancer is abnormal vaginal bleeding — especially bleeding after menopause. Other possible signs include pelvic pain, pain during intercourse, painful urination, unexplained weight loss, and, in later cases, a palpable pelvic mass.
Recognizing early signs of uterine (endometrial) cancer improves the chance of prompt diagnosis and effective treatment. Many symptoms overlap with less serious conditions, but certain red flags deserve immediate evaluation:
- Abnormal Vaginal Bleeding: The hallmark symptom — any bleeding after menopause, or heavy/intermittent bleeding between periods in premenopausal women, should prompt urgent assessment.
- Pelvic Pain or Pressure: Persistent cramping or aching in the lower abdomen or back that does not resolve with usual treatments.
- Pain During Intercourse (Dyspareunia): New or worsening pain with sex can reflect changes in the uterus or surrounding tissues.
- Painful or Frequent Urination: If a tumor presses on the bladder, urinary symptoms may occur — though urinary tract infections are a more common cause.
- Unexplained Weight Loss or Fatigue: Systemic symptoms can appear in advanced cases and warrant investigation.
- Pelvic Mass or Swelling: A noticeable lump or fullness in the pelvis may indicate later-stage disease.
When to see a doctor: any postmenopausal bleeding, bleeding between periods, or new pelvic pain — get evaluated by a gynecologist. For international or second-opinion consultations, bring your pathology report, imaging (ultrasound/CT/MRI), and records of any prior tests or treatments to help clinicians assess your case quickly.
What causes uterine cancer and who is at risk?
Uterine cancer begins when genetic mutations allow abnormal cells in the endometrium (the lining of the uterus) to grow uncontrollably. While many cases have no single identifiable cause, certain factors increase the likelihood of developing endometrial or other uterine cancers.
Risk factors fall into two categories: non‑modifiable (age, genetics) and modifiable (weight, hormone exposure). Understanding your risk can help guide screening, prevention, and earlier diagnosis.
Common risk factors
- Age: Risk rises with age and most cases occur after menopause.
- Obesity: Excess fat tissue increases estrogen levels, which can stimulate the endometrium and raise uterine cancer risk.
- Hormone exposure: Long-term unopposed estrogen therapy (estrogen without progesterone), early menarche or late menopause, and certain ovarian tumors that produce estrogen increase risk.
- Reproductive history: Never having been pregnant is associated with a modestly higher risk.
- Medications: Tamoxifen (used in breast cancer) can act like estrogen in the uterus and slightly raise risk.
- Genetic syndromes: Lynch syndrome (HNPCC) substantially increases the risk of endometrial and other cancers — genetic counseling/testing is recommended for people with strong family histories.
- Diabetes and metabolic factors: Insulin resistance and related metabolic issues are linked with higher risk.
- Rare types: Uterine sarcomas are less common and arise from muscle or connective tissue rather than the endometrium; their risk profile differs.
What you can do
Modifiable steps that may lower risk include managing weight, controlling diabetes, discussing hormone therapy options with your clinician, and, if indicated, pursuing genetic counseling for hereditary syndromes. If you have risk factors or symptoms (especially postmenopausal bleeding), see a gynecologist for appropriate tests — typically pelvic ultrasound and endometrial biopsy — to obtain an accurate diagnosis.
What are the types of uterine cancer treatments available?
Treatment for uterine cancer commonly centers on surgery (hysterectomy) and may include radiation therapy, chemotherapy, hormone therapy, targeted agents, or immunotherapy depending on the cancer type, stage, and patient factors.
Choosing among uterine cancer treatment options depends on whether the tumor arises from the endometrium (endometrial cancer) or from other uterine tissues (for example, uterine sarcoma), the stage, molecular features, and the patient’s overall health and priorities (including fertility preservation when relevant).
Quick reference: Early-stage endometrial cancers are often treated with surgery alone; intermediate/high‑risk tumors may need adjuvant radiation or chemotherapy; advanced or recurrent disease commonly uses systemic therapy (chemotherapy, targeted therapy, or immunotherapy) and individualized multidisciplinary care.
- Surgery (Hysterectomy): The cornerstone for most uterine cancers is surgical removal of the tumor. Options include:
- Total hysterectomy: Removal of the uterus and cervix.
- Bilateral salpingo‑oophorectomy (BSO): Removal of both fallopian tubes and ovaries is commonly performed with hysterectomy, especially in postmenopausal women.
- Lymphadenectomy / sentinel node mapping: Sampling or removal of pelvic and para‑aortic lymph nodes to assess spread.
- Minimally invasive approaches: Laparoscopic or robotic surgery is often used for early‑stage disease and offers smaller incisions and quicker recovery; open surgery may be needed for large or advanced tumors.
- Fertility‑sparing options: In select, carefully staged early cases (young women with low‑grade, early endometrioid tumors), hormonal management with progestin therapy and close surveillance may be considered — discuss risks with a gynecologic oncologist.
- Radiation therapy: Uses high‑energy rays to destroy cancer cells; often used after surgery (adjuvant) to reduce local recurrence or as definitive therapy in non‑surgical candidates.
- External beam radiation therapy (EBRT): Delivered from outside the body to the pelvis.
- Brachytherapy (vaginal cylinder or intracavitary): Internal radiation placed close to the tumor bed; commonly used for endometrial cancers to lower vaginal cuff recurrence.
- Chemotherapy: Systemic drugs that kill rapidly dividing cancer cells; most often used for advanced-stage disease, high‑risk histologies, or recurrence. Common regimens may include carboplatin and paclitaxel, but choices vary by case and emerging evidence.
- Hormone therapy: For hormone‑receptor‑positive endometrial cancers, progestins, aromatase inhibitors, or other endocrine agents can control disease growth, and are sometimes used in low‑grade or metastatic settings to avoid chemotherapy.
- Targeted therapy: Drugs that attack molecular vulnerabilities in cancer cells. Targeted agents are chosen based on tumor testing (for example, alterations detected on genomic profiling). Side‑effect profiles differ from chemotherapy and are drug‑specific.
- Immunotherapy: Checkpoint inhibitors may benefit tumors with mismatch repair deficiency (dMMR) or high microsatellite instability (MSI‑H). These newer therapies are important options for certain advanced or recurrent endometrial cancers and require molecular testing of the tumor.
Your multidisciplinary team (gynecologic oncologist, radiation oncologist, medical oncologist, and supportive‑care specialists) will recommend a personalized plan based on endometrial cancer stage, histologic type (including distinction from uterine sarcoma), molecular markers, overall health, and patient preferences. Ask your team about expected benefits, likely side effects, and recovery timelines for each option.
Who is eligible for uterine cancer treatment?
Most women diagnosed with uterine cancer are candidates for treatment. Eligibility and the specific treatment plan depend on the cancer’s stage and type (endometrial carcinoma vs. rarer uterine sarcomas), the patient’s overall health, and individual goals such as fertility preservation.
A confirmed diagnosis typically leads to a personalized treatment recommendation. Factors your medical team will consider include:
- Cancer stage: Early-stage disease confined to the uterus often requires surgery alone; higher stages may need combined modality therapy (surgery plus radiation and/or chemotherapy).
- Cancer type and biology: Endometrial cancers and uterine sarcomas have different treatment protocols; molecular testing (e.g., MSI/dMMR) can guide targeted or immunotherapy choices.
- Overall health and comorbidities: Conditions such as heart disease, diabetes, or poor pulmonary function may affect surgical candidacy and require tailored approaches.
- Patient preferences: Desire to preserve fertility, tolerance for potential side effects, and personal values are important in choosing between surgery, hormone therapy, or other options.
- Age: Age itself is not an absolute barrier, but older patients may need extra evaluation to manage comorbidities during treatment.
Typical pre‑treatment workup
Before finalizing eligibility and a treatment plan, clinicians will usually order imaging (pelvic ultrasound, CT or MRI as needed), an endometrial biopsy to confirm diagnosis, and blood tests to assess fitness for surgery or systemic therapy.
Checklist before seeking treatment (especially abroad)
- Obtain and bring copies of pathology reports and, if possible, slides or reports from the pathology lab.
- Collect recent imaging studies (ultrasound, CT, MRI) on CD or digital files and operative notes if prior surgery was performed.
- Prepare a medication list and records of other health conditions (cardiac, diabetes, etc.).
- Ask prospective centers for surgeon CVs, annual case volumes, accreditation, and an itemized treatment plan and quote.
Even in complex or recurrent cases, multidisciplinary care can often offer meaningful treatment options to control disease and improve quality of life. If you plan to seek a second opinion or treatment abroad, request your full diagnostic package from your current provider to speed evaluation by the foreign team.
What is the recovery time and what to expect after uterine cancer treatment?
Recovery after uterine cancer treatment varies by modality. After surgery most patients stay in hospital for a few days and often feel back to baseline within 4–8 weeks; recovery from radiation or chemotherapy is typically more gradual, with fatigue and other side effects resolving over several months.
Knowing what to expect after uterine (endometrial) cancer treatment helps you plan practical needs (help at home, time off work, travel) and recognize symptoms that need prompt attention. Below are typical timelines and common issues by treatment type.
- After surgery (hysterectomy):Hospital stay: Typically 2–7 days depending on whether the procedure was minimally invasive (laparoscopic/robotic) or open.
- Initial recovery: Expect incision pain, fatigue, and limited mobility for the first 2–4 weeks; avoid heavy lifting and strenuous activity during this time.
- Full recovery: Most people return to routine activities within 4–8 weeks; emotional recovery (mood changes, body image, sexual health) can take longer and may benefit from counseling or support groups.
- When to seek care: Fever, increasing redness or drainage at the incision, sudden worsening pain, shortness of breath, or calf swelling (possible blood clot) require prompt medical attention.
- After radiation therapy:Common side effects: Fatigue, skin irritation in the treated area, vaginal dryness, and temporary bowel or bladder changes. These often peak during treatment and gradually improve over weeks to months.
- Long-term issues: Some patients may experience vaginal stenosis or chronic bowel changes; pelvic physiotherapy and vaginal dilator programs can help reduce complications.
- After chemotherapy:Common side effects: Fatigue, nausea, hair loss, mouth sores, and lower immunity are frequent but usually manageable with supportive care.
- Recovery: Blood counts and energy often take weeks to months to recover after finishing chemotherapy; some effects (peripheral neuropathy, cognitive changes) can persist longer.
- Recovery checklist (practical tips):Arrange help at home for the first 1–2 weeks after surgery (meals, errands).
- Plan travel carefully—many clinicians advise delaying long flights for several weeks after major surgery; confirm clearance with your surgeon or oncologist.
- Keep an emergency contact and a list of warning signs that require immediate care.
- Discuss rehabilitation resources (pelvic physiotherapy, lymphedema services) and sexual-health counseling before or during recovery.
Regular follow-up is essential to monitor for recurrence and manage long‑term effects. Many patients find peer support groups and mental‑health counseling helpful for emotional recovery. If you are considering treatment abroad, confirm the expected recovery timeline with the treating team and plan local follow‑up with your home physicians to ensure continuity of care.
What are the risks and side effects of uterine cancer treatment?
All uterine cancer treatments carry potential risks and side effects. Surgery can involve bleeding and infection; radiation may cause fatigue and bowel or bladder changes; chemotherapy commonly causes nausea and low blood counts. Understanding expected effects helps you prepare and ask the right questions about supportive care.
Knowing the likely risks of uterine (including endometrial) cancer treatment lets you weigh benefits and plan mitigation strategies. Below are common and less common effects by treatment type, plus practical management tips.
- Surgery (hysterectomy):Common risks: Bleeding, wound infection, anesthetic reactions, and blood clots.
- Specific concerns: Damage to nearby organs (bladder, bowel), lymphedema after lymph node removal, and surgical menopause if ovaries are removed.
- Management: Early mobilization, DVT prophylaxis, wound care instructions, and referral to lymphedema or pelvic‑floor services when needed.
- Radiation therapy (external beam and brachytherapy):Short‑term effects: Fatigue, skin irritation in the treated area, vaginal dryness, and temporary bowel or bladder changes such as diarrhea or increased urinary frequency.
- Long‑term effects: Vaginal stenosis (narrowing), persistent bowel changes (rare chronic diarrhea or rectal bleeding), and possible bladder issues. Pelvic physiotherapy and dilator programs can help prevent or manage vaginal stenosis.
- Management: Skin care guidance, dietary adjustments for bowel symptoms, vaginal moisturizers/dilators, and coordination with pelvic rehab specialists.
- Chemotherapy:Common: Fatigue, nausea, hair loss, mouth sores, decreased appetite, and increased risk of infection due to low blood counts; some drugs cause peripheral neuropathy (numbness/tingling).
- Serious but less common: Bone marrow suppression (anemia, neutropenia), kidney or heart toxicity with certain agents — clinicians monitor blood work and organ function during treatment.
- Management: Anti‑nausea medications, growth‑factor support for low blood counts, dose adjustments, and rehabilitation for neuropathy when needed.
- Hormone therapy & targeted therapy:Hormone therapy: Hot flashes, vaginal dryness, mood changes, and a small increased risk of blood clots with some agents.
- Targeted agents: Side effects vary by drug but can include skin rash, diarrhea, high blood pressure, and liver enzyme abnormalities; targeted therapies are selected based on tumor testing.
- Management: Routine labs to monitor liver and kidney function, blood‑pressure control, dermatology support for rashes, and symptomatic treatments tailored to each agent.
- Practical tips for managing side effectsDiscuss supportive‑care measures up front (antiemetics, growth factors, pain management, nutritional support).
- Ask about referrals to pelvic‑floor therapy, lymphedema clinics, or oncology rehabilitation for long‑term effects.
- Keep a symptom diary to share with your care team and report concerning changes promptly (heavy bleeding, severe pain, fever, signs of infection).
Your oncology team will explain which side effects are most likely in your case and how they will monitor and treat them. Many side effects are temporary or manageable with supportive care; some rare long‑term effects require ongoing management. If you plan treatment abroad, confirm that the treating center has protocols for managing complications and a clear post‑treatment follow‑up plan with your local physicians.
Worldwide Cost Comparison for Uterine Cancer Treatment
The cost of uterine cancer care varies widely around the world. In high‑cost health systems, a surgical package with hospitalization and initial follow‑up can run into the tens of thousands of dollars; many medical tourism destinations offer comparable clinical services at substantially lower prices. The figures below are illustrative ranges for a typical package (hysterectomy with lymph node assessment and short post‑op stay) — exact quotes depend on the hospital, surgeon, extent of surgery, and any additional treatments (chemotherapy, radiation, targeted therapy).
Patients searching for “uterine cancer treatment abroad cost” often compare total expected expenses, including surgeon and hospital fees, anesthesia, basic post‑operative care and a short inpatient stay. Note: items often NOT included in headline prices are chemotherapy cycles, extended ICU care, additional imaging, or long‑term follow‑up — always request an itemized quote and ask what is and isn’t covered.
| Country Estimated Cost Range (USD) Notes | ||
| United States | $40,000 – $120,000+ | Advanced care and high procedural costs; out‑of‑pocket expense varies widely with insurance. |
| United Kingdom | $35,000 – $80,000+ | NHS covers residents; private care prices can be high for international patients. |
| Turkey | $18,000 – $45,000 | Modern facilities, many JCI‑accredited centers offering robotic surgery and multidisciplinary care. |
| Mexico | $15,000 – $35,000 | Closer for North American patients; quality care at lower prices, but verify accreditation and surgeon experience. |
| India | $12,000 – $30,000 | World‑class hospitals in major cities offer cost‑effective care; ensure you review surgeon volumes and outcomes. |
| Thailand | $15,000 – $38,000 | Accredited private hospitals with strong patient services and good value for complex procedures. |
*These costs are estimates for illustrative purposes and may not reflect current local pricing or the exact scope of care you require. Always request an itemized, written quote that specifies what is included (surgeon fees, hospital bed, anesthesia, basic post‑op care) and what may be extra (chemotherapy cycles, advanced imaging, extended stays, complications).
- Practical advice:Ask clinics for an itemized quote and expected length of stay.
- Factor in travel, accommodation for family, recovery time, and potential costs for follow‑up at home.
- Ensure the quote covers contingency plans for complications and whether the center offers international patient coordination and post‑discharge follow‑up.
Why consider uterine cancer treatment abroad?
Seeking uterine cancer care overseas can offer cost savings, access to specialized technologies or clinical trials, shorter wait times, and a patient‑centered experience with international patient services. However, it’s important to balance benefits against practical considerations like continuity of care, travel risk, and insurance coverage.
Patients often explore “uterine cancer treatment abroad” for several reasons. Below are common advantages — and key downsides to weigh — to help you make an informed decision.
Potential benefits
- Cost savings: Lower procedure and facility fees can make surgery, radiation, or combined treatment more affordable for patients without robust insurance.
- Access to advanced technology: Some centers abroad provide robotic surgery, specialized brachytherapy suites, or molecular testing that guide targeted therapy and immunotherapy choices.
- Shorter wait times: Faster scheduling for consultations and procedures can be crucial when time is a factor.
- Enhanced patient services: Many international hospitals offer concierge support, language assistance, and coordinated logistics for travel and recovery.
Potential downsides
- Continuity of care: Post‑operative follow‑up and management of complications require careful coordination between the treating center and your local doctors.
- Travel risks: Long flights soon after major surgery or during systemic therapy can increase risks such as blood clots or infection.
- Insurance and liability: Coverage for complications or readmission may be limited; malpractice and legal recourse differ by country.
- Variability in outcomes: Quality varies by hospital and surgeon—verify accreditation, surgeon volume, and outcome data rather than relying on marketing alone.
Questions to ask foreign providers
- Is the facility internationally accredited (e.g., JCI)? Ask for accreditation details.
- How many uterine cancer surgeries does the surgeon perform yearly, and what are their complication rates?
- What exactly is included in the cost estimate (surgeon fees, hospital stay, anesthesia, basic post‑op care)? What is excluded?
- Do you offer molecular testing to guide targeted therapy or immunotherapy, and can you coordinate post‑discharge follow‑up with my local team?
- What contingency plans and costs exist if complications occur or additional treatment is needed?
When considering treatment abroad for endometrial or other uterine cancers, weigh these pros and cons, request detailed documentation (surgeon CV, accreditation, outcome data), and plan for seamless handover to local care after you return. A balanced approach helps you maximize benefits while minimizing risks.
Which countries offer the best value for uterine cancer treatment?
For many patients seeking affordable, high‑quality care for uterine cancer (most often endometrial cancer), countries such as Turkey, Mexico, India, Thailand, and South Korea frequently offer strong value — combining accredited hospitals, experienced specialists, and lower overall costs compared with some Western health systems.
When evaluating “top destinations for uterine cancer care,” consider each country’s strengths (technology, cost, patient services) and practical factors like visa rules and ease of follow‑up. Below are concise country profiles and what they commonly offer for uterine cancer patients.
- Turkey: Many Turkish centers (especially in Istanbul and Ankara) are JCI‑accredited and offer multidisciplinary uterine cancer care, including minimally invasive and robotic surgery, advanced radiation techniques, and comprehensive post‑op services. Wait times are often short and international patient coordination is well established.
- Mexico: Popular with North American patients due to proximity and lower travel burden. Cities such as Guadalajara, Mexico City, and Tijuana have modern hospitals with experienced gynecologic oncologists; costs tend to be substantially lower than in the U.S., but verify facility accreditation and surgeon experience.
- India: A leader in cost‑effective cancer care, India’s major cancer centers in Delhi, Mumbai, Chennai and Bangalore provide world‑class surgical oncology, targeted therapies, and advanced radiation at very competitive prices. Many physicians have international training; ensure you review outcomes and hospital accreditation.
- Thailand: Known for excellent private hospitals and strong patient services (concierge, English-speaking staff). Bangkok centers often combine high-quality perioperative care, comfortable recovery facilities, and efficient international patient programs.
- South Korea: While sometimes more expensive than other Asian destinations, South Korea is recognized for technological excellence (robotic surgery, precision oncology) and fast, efficient care — attractive for patients prioritizing cutting‑edge surgical and diagnostic techniques.
Caveats and practical tips: accreditation and surgeon volume vary by hospital — ask for JCI or equivalent accreditation, surgeon case numbers for hysterectomy/gynecologic oncology, complication rates, and examples of outcomes. Also confirm visa requirements, typical wait times, and how post‑discharge follow‑up will be handled with your local providers.
What to expect when traveling for uterine cancer treatment abroad?
Expect a coordinated process that begins with virtual consultations and documentation review, moves through travel logistics and on‑site diagnostics, proceeds to treatment and inpatient recovery, and finishes with a planned handover for follow‑up care at home.
Medical tourism for uterine (including endometrial) cancer can be an effective option when planned carefully. Below is a practical timeline and checklist so you know what to prepare and when to expect each step.
Typical timeline (example for a surgical package)
- Weeks −4 to −2 (Initial planning): Gather and send your medical records — pathology report, biopsy slides (if available), imaging (ultrasound, CT or MRI), operative notes, and test results. Schedule a remote consultation to review the case and receive a proposed treatment plan and itemized quote.
- Weeks −2 to 0 (Logistics): Arrange visa, flights, and accommodation. Confirm travel insurance coverage and discuss any travel restrictions with your care team (e.g., timing relative to chemotherapy or major surgery).
- Arrival & pre-op (Day 0–3): Clinic will usually perform on‑site diagnostics to confirm staging (repeat or supplementary imaging, labs) and finalize consent and scheduling.
- Treatment & inpatient recovery (Day 1–14): Undergo surgery, radiation, or other planned therapy; typical hospital stay for hysterectomy ranges from 2–7 days depending on approach. Plan for initial recovery in your lodging near the clinic after discharge if advised.
- Recovery & return (Weeks 1–6+): You will receive discharge instructions and a post‑op care plan. Travel home once medically cleared — many centers require a minimum recovery period before long flights (confirm with the treating team). Arrange local follow‑up with your home physicians.
Essential documents to prepare
- Pathology report and, if possible, slides or digital pathology images.
- Recent imaging (pelvic ultrasound, CT, MRI) in DICOM format or on CD/DVD and radiology reports.
- Operative notes, prior treatment records, medication list, allergies, and comorbidity details (heart, diabetes, etc.).
- Insurance information and a signed medical‑release form authorizing records transfer.
Practical tips & risk mitigation
- Ask the treating center how long they recommend you stay post‑op before flying home — many advise waiting several weeks depending on the procedure.
- Confirm that the facility can manage complications and that contingency plans (and costs) are clear in writing.
- Arrange communication between the foreign team and your local gynecologist/oncologist to ensure continuity of care and clear follow‑up instructions.
- Pack a recovery kit: medications, compression stockings (to reduce clot risk during travel), a list of emergency contacts, and printed copies of all medical documents.
Reputable medical tourism facilitators and international patient offices can coordinate logistics (appointments, transfers, translation), but always verify clinical credentials, accreditation, and obtain a detailed, itemized treatment plan and quote. If you’re undergoing radiation therapy or chemotherapy, check specific travel timing recommendations with your oncology team to minimize health risks.
How to ensure safety and quality of uterine cancer treatment abroad?
Prioritize accredited hospitals, experienced gynecologic oncologists, transparent communication, and a clear post‑operative plan. Rigorous vetting reduces risk and helps ensure high‑quality care for uterine and endometrial cancers when seeking treatment internationally.
Choosing a safe facility abroad takes due diligence. Use the checklist and sample questions below to verify standards, surgical experience, and continuity of care before committing to treatment.
Verification checklist
- Accreditation: Confirm international accreditation such as JCI or equivalent national/ISO certifications to verify hospital safety and quality systems.
- Surgeon & team credentials: Request surgeon CVs, board certifications, annual case volumes for gynecologic oncology procedures (e.g., hysterectomy, lymphadenectomy, robotic cases), and outcomes if available.
- Facility standards & technology: Verify availability of necessary services (robotic surgery, advanced radiation therapy, ICU, pathology and molecular testing) and infection‑control practices.
- Patient outcomes & reviews: Look for objective indicators (published outcomes, peer referrals) and consistent patient testimonials; be cautious of only promotional stories.
- Transparent costs & contracts: Obtain an itemized written quote that states what is included (surgeon fee, anesthesia, hospital stay, basic post‑op care) and what is excluded (chemotherapy cycles, extended rehabilitation, complications).
- Post‑operative and follow‑up plan: Ensure there is a documented plan for post‑discharge care, communication with your local doctors, and handling complications (including costs and timelines).
Sample questions to ask providers
- How many uterine cancer surgeries (and robotic hysterectomies, if applicable) does this surgeon perform annually?
- Can you provide complication and readmission rates for the proposed procedure?
- Is the pathology/molecular testing done in‑house, and will I receive copies of pathology slides/reports?
- What exactly is included in the quoted price and what would trigger additional charges?
- How will you coordinate post‑treatment follow‑up with my local care team, and who is the point of contact for complications after I return home?
Additional safeguards
- Get at least two independent opinions if feasible, especially for complex cases or when recommended treatments differ from standard guidelines.
- Ensure the facility will share medical records electronically and provide a clear discharge summary and survivorship care plan for your local physicians.
- Confirm the facilitator’s role: reputable coordinators arrange logistics and vet partners but do not replace clinical decision‑making — clinical responsibility rests with the treating physicians and hospital.
Being thorough with accreditation checks, clinician credentials, outcome data, and a documented post‑op plan will help you find safe, high‑quality care for uterine or endometrial cancer abroad. Don’t hesitate to request documentation and time to review it with a trusted local specialist before proceeding.
What are patient success stories from uterine cancer treatment abroad?
Many patients report positive outcomes after seeking uterine cancer care overseas, including remission, improved quality of life, and relief from financial burden when comparing international treatment packages to domestic costs. These accounts commonly highlight timely access to surgery, advanced techniques (such as robotic hysterectomy), and attentive post‑op support.
Patient stories can be encouraging, but remember they are anecdotal. Look for objective information (aggregate outcomes, hospital accreditation, surgeon volumes) in addition to testimonials. Typical themes in verified success narratives include:
- Successful remission: Patients with early‑stage endometrial cancer who received prompt surgery abroad (including minimally invasive or robotic approaches) often report long disease‑free intervals and return to normal life.
- Improved quality of life: Faster access to treatment and less invasive surgery can shorten recovery and reduce long‑term effects, contributing to better physical and emotional recovery.
- Positive patient experience: Many international centers provide strong patient‑centered services—concierge support, language assistance, and coordinated care—that patients cite as enhancing their overall experience during a stressful time.
- Financial relief: Patients without adequate insurance report that lower procedure and hospital fees abroad reduced financial strain, allowing them to focus on recovery rather than costs.
- Access to innovation: Some patients travel for specific therapies, molecular testing, or clinical trials (for example, targeted therapy or immunotherapy for certain tumor profiles) that were not available locally.
- How to evaluate testimonialsAsk whether outcomes are typical or represent exceptional cases; request anonymized outcome statistics if available.
- Request references or patient‑reported outcome data and confirm the treating surgeon and hospital details.
- Balance testimonials with independent indicators (accreditation, published outcomes, peer referrals).
If you’re considering treatment abroad, ask providers for anonymized case summaries or aggregated data that show remission and complication rates for similar uterine cancer cases. That evidence, combined with verified accreditation and surgeon experience, gives a clearer picture than testimonials alone.
Take the Next Step with DGS Healthcare
Ready to explore safe, accredited options for treatment abroad? Compare top clinics, review surgeon credentials, and get a free, itemized quote tailored to your uterine cancer care needs with DGS Healthcare.
What to have ready: pathology reports, imaging (ultrasound/CT/MRI), and a summary of prior treatments. Expect a response within 48–72 hours. Your records are handled confidentially.
Medical disclaimer: information provided by facilitators does not replace professional medical advice. Consult your local provider before traveling for major surgery. DGS Healthcare and partner clinics will request necessary medical documentation and will outline what the quote includes and any exclusions.
